Medical/Patient Care
Questions pertaining to medical or patient care
Any contraindication treating patient with patent foramen ovale?
Posted: 5/25/23
Q: Any contraindication treating patient with patent foramen ovale?
A: In the general population 30% of individuals have a PFO. Individuals with a PFO have a slightly increased risk of decompression sickness (DCS). However, the risk of DCS for a patient undergoing hyperbaric oxygen treatment is zero. Thus, for patients undergoing HBO2 treatment the presence of a PFO is irrelevant.
What is the main concern or danger with a systolic blood pressure below 100 pre HBO treatment assessment?
Posted:11/13/23
Q:
What is the main concern or danger with a systolic blood pressure below 100 pre HBO treatment assessment?
A:
There is nothing magic about a systolic BP less than 100mmHg in the hyperbaric environment. Various authors have studied the impact of BP as the result of hyperbaric treatments. We know that HBO2 causes arteriolar constrictions and increased afterload, sometimes leading to the occurrence or worsening of CHF. For most patients, the changes are negligible. But for a patient with hypotension in the chamber, the tendency is for a BP increase not a decrease.
I am not sure where you got this guidance. I would like to know for future reference. The thinking, I believe, arises out of caution because 100 mmHg systolic is a fairly low pressure and may be due to sepsis or blood loss. More than anything, I believe whoever authored this policy was trying to alert the treating HBO2 doctor that the patient may be having significant intercurrent disease symptoms and should be stabilized before going into the chamber.
There is a subset of slight young women who characteristically will run blood pressures like this. It is therefore important to get the patient’s history or check previous medical trecords to determine if this is a normal and usual pressure for your patient.
John J. Feldmeier, D.O.
Does a patients A1C need to be below a certain number before HBO tx is beneficial?
Posted: 6/20/24
Q: Does a patients A1C need to be below a certain number before HBO tx is beneficial?
A:
No. The question is if the email is referencing the wound care literature, which is split between those who feel better control equates to better outcomes and those who believe that all patients deserve a trial.
If the question is referencing the requirement for DFU and HBOT, then the question is more about documenting an A1C and then referring them to a nutritionist/PCP for counseling and intervention. There is a schism even within the diabetes community as to what constitutes good control; it varies depending upon the age of the patient and the co-morbidities.
https://diabetesjournals.org/care/article/46/Supplement_1/S216/148044/13-Older-Adults-Standards-of-Care-in-Diabetes-2023
Whether or not they have significant autonomic dysfunction and can sense hypoglycemia is a major risk factor that needs to be addressed.
There are multiple examples in the literature where A1C and outcomes are not linked in the hyperbaric medicine space.
Helen Gelly, MD, FUHM, FACCWS, UHM/ABPM
Thank you.
We have a patient with recent bilateral mastectomy and tissue expanders. What are the requirements if expanders are filled with air vs. saline for treating in hyperbaric? This question is urgent as the indication is flap failure.
Posted 7/11/24
Q: We have a patient with recent bilateral mastectomy and tissue expanders. What are the requirements if expanders are filled with air vs. saline for treating in hyperbaric? This question is urgent as the indication is flap failure.
A:
Patients referred for acute vascular ischemia of the breast tissue following mastectomy, including nipple areola complex ischemia, are referred for hyperbaric oxygen treatment (HBO2) in an attempt to arrest the ischemia and hypoxia produced from the extensive dissection necessary during the mastectomy.
First, tissue expanders used in breast reconstruction are almost always filled with saline. Here are some key points regarding the use of saline versus air:
- Saline: The standard practice is to fill tissue expanders with saline. Saline is preferred because it is not compressible under pressure changes, such as those experienced during hyperbaric oxygen therapy and air travel. This stability mitigates risk best with saline-filled expanders and more predictable as fluid does not respond to pressure changes in a hyperbaric chamber, pressurized aircraft, or moving from areas of high pressure to low pressure and vice versa.
- Air: Filling tissue expanders with air is extremely uncommon. Air-filled expanders are susceptible to compression and expansion with changes in atmospheric pressure posing risks in environments such as hyperbaric chambers, during flights in pressurized aircraft, and changes in atmospheric pressure from location to location. The use of air-filled expanders is typically limited to temporary situations or specific clinical scenarios where immediate, short-term expansion is needed, and the patient is not exposed to significant pressure changes.
Clinical Practice: Tissue expanders are usually filled with saline to mitigate risk and better ensure patient safety and optimal outcomes in various clinical situations and environmental pressure change.
To safely proceed with hyperbaric oxygen treatment and prevent worsening ischemia, it is recommended that:
- Tissue expander volume should be reduced: Remove enough saline (or air) from the expanders to decrease stress and tension on tissue and suture lines. This reduces pressure on the breast tissue, which could be contributing to the ischemia.
- If volume reduction is not possible: Remove the expanders as soon as feasible to alleviate pressure on the surrounding vessels post-mastectomy.
This approach ensures the patient can undergo HBO2 while minimizing the risk of exacerbating the ischemia.
In cases where tissue expanders are inserted following a bilateral mastectomy, where significant tissue removal has occurred, the immediate post-operative filling of tissue expanders requires careful consideration on the part of the plastic surgeon:
- Immediate Post Operative Filling: Typically, tissue expanders are filled with a small amount of saline at the time of placement to maintain their position and avoid collapse. This initial fill should be minimal to reduce the risk of excessive pressure on the newly operated tissue.
- Gradual Expansion: The expansion process should be gradual and carefully monitored. Regular follow-ups with the surgeon are necessary to incrementally increase the fill volume, allowing the tissue to stretch slowly and reducing the risk of complications such as ischemia or undue pressure on the tissue.
- Consideration of Ischemia Risk: In patients at risk of ischemia, particularly those referred for hyperbaric oxygen treatment, it may be prudent to delay significant filling of the expanders until the risk of ischemia has been thoroughly assessed and managed.
- Customizing to Patient Needs: The decision should be individualized based on the patient's condition, the extent of tissue removal, and the surgeon’s judgment. Close monitoring for signs of ischemia or other complications is essential.
In summary, while tissue expanders can be initially filled post-operatively, the volume should be minimal, with careful and gradual expansion thereafter. The specific approach should be tailored to the patient's needs and clinical situation, particularly if there is a significant risk of ischemia or ischemia becomes apparent. This response addresses the concerns about using HBO2 treatment with tissue expanders and provides guidelines for managing such cases.
Owen ONeill, MD, MPH, FUHM, FACHM
Taxotere and HBO2: Are there known complications or contraindications?
Posted; 7/23/24
Q:
Taxotere and HBO2: Are there known complications or contraindications?
A:
Literature Search: A literature search was accomplished by me. No specific publications were found that reported unexpected or unexpectedly severe complications of Taxotere when given concurrently with hyperbaric oxygen.
Introduction: Taxotere is a member of the class of chemotherapy drugs called Taxanes, which also includes Taxol. It works to inhibit cancer cell mitosis by interfering with the tubules that participate in that part of mitotic reproduction.
The Tables below give the common and the severe complications caused by this drug.
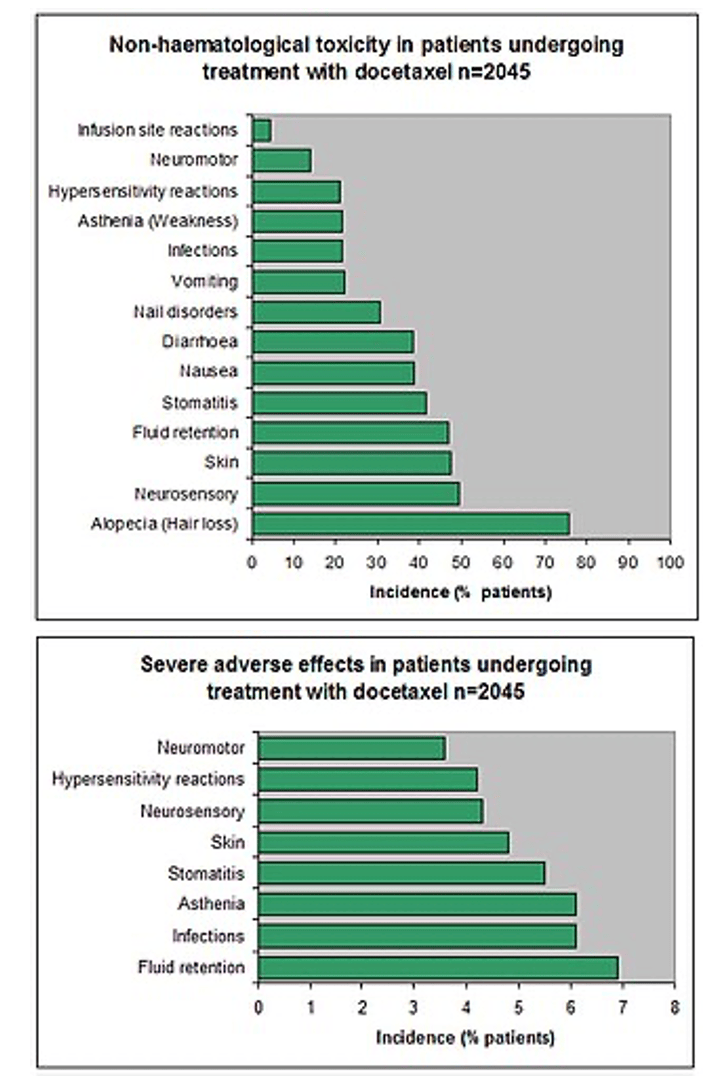
Note, these tables were taken from the Wikipedia write up of Taxotere.
Of note, GI effects are common, and when patients are treated in the chamber, diarrhea may occur and be difficult to manage in that environment.
Also, fluid retention is reported as a potentially severe complication which could increase the likelihood of CHF and flash pulmonary edema which as you know can occur in the chamber. Patients should be checked daily for fluid retention and respiratory deterioration.
Finally , a lung complication abbreviated DPLD (diffuse parenchymal lung disease) can be a fatal pulmonary complication of Taxotere. Patients should be carefully monitored for this complication.
There are no specific complications that would be expected to be exacerbated specifically due to high doses of oxygen given while the patient is being treated with Taxotere.
Since there is no published experience for the interaction of the 2 modalities, knowledge of the kinetics of the drug can be helpful. Three different serum half lives are reported for the drug. The longest of these is 12.2 hours. It is commonly administered by IV infusion every 3 weeks. After the passage of 5 half lives (5 X 12.2 hours) or 61 hours ( just a little over 2 days), the concentration of the drug will have fallen to about 3% of the maximum dose. I would recommend that a short interruption of the HBO2 occur to allow clearance of the drug to that level. If Taxotere is given on a Friday, by Monday, the levels will be below 3%. By reducing the drug concentration to such a low level, the potential for interactions of the riuch oxygen environment and the drug should be minimized.
As always, the decision to treat a patient with HBO2 is the purview of the physician who will be in charge of the treatment and has seen the patient in person and given an informed consent.
John J. Feldmeier, D.O.
Can you offer any information on an HBO treatment protocol for livedoid vasculopathy. There are a few case studies out there ranging from 1.4 ATA to 2.5 ATA for 1 hour, six day per week and all with similar conclusions of total wound closer and complete resolution of pain with no recurrence of ulcers after 6 to 8 month follow up.
Posted: 8/2/24
Q: Can you offer any information on an HBO treatment protocol for livedoid vasculopathy. There are a few case studies out there ranging from 1.4 ATA to 2.5 ATA for 1 hour, six day per week and all with similar conclusions of total wound closer and complete resolution of pain with no recurrence of ulcers after 6 to 8 month follow up.
A:
Please note that at the present time, the treatment of Livedoid vasculitis and certain other hypoxic wounds are not recognized as approved indications at this time.
A literature search was accomplished in an effort to determine whether there was any published material to provide guidance for responding to this question. There were very few articles that addressed this issue. Those that were available were case reports or small case series. Just as the individual who posed this question, I found when the pressures for treatment were reported, they varied from 1.45 ATA to 2.8 ATA. The paper advocating 1.45 ATA comes from Costa Rico by Herrera-Sanchez et al (Medicina (Buenos Aires) 2022 82:613-6.) Many of the Mild Hyperbaric documents advocate these low pressures primarily based on the false premise that treatments at this pressure are inherently safer and equally effective as standard pressures advocated by mainstream hyperbaric oxygen advocates. The Indications Manual 15th Edition, edited by Dr. Enoch Huang, now clearly defines clinical hyperbaric oxygen treatment as treatment occurring between 2.0 to 3.0 ATA. The chapter in this book by Huang et al discusses the mechanisms of hyperbaric oxygen in the treatment of chronic hypoxic wounds. The importance of adequate oxygen delivery and its impact on several biochemical events required to achieve a closed wound, including angiogenesis in the wound, are summarized here.
Transcutaneous oxygen assessment can be of use when selecting a treatment pressure. In diabetic foot ulcers, in a series of over 1000 patients, Fife et al have shown that transcutaneous measurements exceeding 200 mmHg in the chamber during treatment are needed to predict an improved likelihood of healing (Fife CE, Smart DR, Sheffield PJ, Hopf HW, Hawkins G, Clarke D. Transcutaneous oximetry in clinical practice: consensus statements from an expert panel based on evidence. Undersea Hyperb Med. 2009 Jan-Feb;36(1):43-53. PMID: 19341127. These patients were treated at 2.0 and 2.4 ATA. Likewise, Sheffield and co-authors had reported that transcutaneous measurements done with a challenge of 100% oxygen accomplished at ground level demonstrated a better outcome when this level was greater than or equal to 150% of the value obtained on ground-level air when the raw value exceeded 35 mmHg (Hyperbaric Oxygen Treatment Of Hypoxic Wounds Sheffield PJ, Dietz D, Posey KI, Sheffield JC, *Bakken B. Nix Wound Healing Center, San Antonio, Texas 7820).
Admittedly, these publications were for diabetic foot ulcers, not livedoid vasculitis ulcers. However, I believe it is widely accepted that the successful treatment of livedoid ulcers requires the delivery of adequate oxygen pressures to carry out the numerous steps involved in healing hypoxic wounds, similarly to diabetic ulcers. It should be noted that most of the reviewed case reports and small series employed 2.5 ATA for their hyperbaric oxygen treatments.
Therefore, my preference and advice to the individual in selecting treatment pressures is to continue to employ pressures of 2.0 to 2.5 ATA for which there is over than 50 years of experience.
John JH. Feldmeier, D.O.
