Item Approval
Is it safe to allow "glass" eyes in the chamber?
Posted 3/17/2021
Q:
Is it safe to allow "glass" eyes in the chamber?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Medical Director and Safety Director of your facility.
The UHMS HBO2 Safety Committee would advise that the Safety Director and Medical Director use caution when evaluating this item for risk, as there may be more risk than is obvious to you. We suggest that your admittance of this item into a hyperbaric environment be dependent upon the construction of the prosthesis (hollow, solid or porous; Integrated or non-integrated) and the patient’s level of comfort and consent with the potential risks involved. If there is any doubt about the construction of the ocular prosthesis, and the item can be easily removed, the UHMS HBO2 Safety Committee recommends removing the ocular prosthesis.
There is a single published study “Diving and Hyperbaric Ophthalmology” in the journal, “Survey of Ophthalmology” by Dr. Frank K. Butler, Jr. indicating that hollow orbital implants are contraindicated to diving:
“Diving contraindicated with hollow orbital implants," Reference pgs. 359, 361.
D. ENUCLEATION: “After the convalescent periods recommended in the previous section, diving should be possible after almost any type of eye surgery. One exception is an individual who has undergone enucleation
and who has a hollow implant. There are reports of pressure-induced collapses of hollow silicone orbital implants at depths as shallow as 10 feet.“’ A hollow glass implant was also tested and did not implode at a maximum test depth of 115 feet, but diving with hollow glass implants could not be recommended on the basis of this one test. Individuals with hollow orbital implants should not dive."
You may also consider that there are integrated implants that are more complex. We would caution that you contact the ophthalmologic surgeon prior to considering allowance in a hyperbaric environment:
The porous nature of integrated implants allows fibrovascular ingrowth throughout the implant and thus also insertion of pegs or posts. Because direct mechanical coupling is thought to improve artificial eye motility, attempts have been made to develop so-called 'integrated implants' that are directly connected to the artificial eye. Historically, implants that directly attached to the prosthesis were unsuccessful because of chronic inflammation or infection arising from the exposed nonporous implant material. This led to the development of quasi-integrated implants with a specially designed anterior surface that allegedly better transferred implant motility to the artificial eye through the closed conjunctiva and Tenon's capsule. In 1985, the problems associated with integrated implants were thought to be largely solved with the introduction of spherical implants made of porous calcium hydroxyapatite. This material allows for fibrovascular ingrowth within several months. Porous enucleation implants currently are fabricated from a variety of materials including natural and synthetic hydroxyapatite, aluminum oxide, and polyethylene.
If your risk assessment uncovers that the object is solid, is not likely to be affected by changes in pressure, and the patient consents, it may be perfectly fine to allow a solid ocular prothesis within the Multiplace or Monoplace hyperbaric environment. This allowance is wholly dependent upon your individual risk assessment performed by the Medical Director and Safety Director of your facility. We would also suggest consulting with the patient’s ophthalmologist to confirm the type of prosthesis. Several Safety Committee members have reported successful treatment of patients with solid (without air spaces) ocular prostheses left in place.
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc. LINK
- Butler Jr, F. K. (1995). Diving and hyperbaric ophthalmology. Survey of ophthalmology, 39(5), 347-366. LINK
- Colen, TP; Paridaens, DA; Lemij, HG; Mourits, MP; Van Den Bosch, WA (2000). "Comparison of artificial eye amplitudes with acrylic and hydroxyapatite spherical enucleation implants". Ophthalmology. 107 (10): 1889–94. LINK
- Custer, PL; Kennedy, RH; Woog, JJ; Kaltreider, SA; Meyer, DR (2003). "Orbital implants in enucleation surgery: a report by the American Academy of Ophthalmology". Ophthalmology. 110 (10): 2054–61. LINK
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is the Cook Doppler wire, disconnected from the Doppler machine, safe to compress in a monoplace environment?
Posted: 3/30/2021
Q:
Is the Cook Doppler wire, disconnected from the Doppler machine, safe to compress in a monoplace environment?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Medical Director and Safety Director of your facility.
The UHMS HBO2 Safety Committee can provide guidance to assist your decision making but cannot endorse a specific product for use in the Monoplace chamber. The Cook doppler wire is also known as a Cook-Swartz Doppler Probe or Ultrasound Probe and is generally used to provide continuous monitoring of microvascular anastomoses.
From a fire safety standpoint, NFPA 99, Chapter 14 (2021) states in 14.2.9.6.1:
“Electrical equipment inside chambers shall be restricted to communications functions and patient physiological monitoring leads.”
and in 14.2.9.6.1.3:
“Patient monitoring leads shall be part of approved electromedical apparatus meeting the requirements in 14.2.9.3.16.”
If the Cook Doppler wire is disconnected from the Doppler Blood Flow Monitoring System and the doppler unit remains outside of the chamber, one would consider the ignition source to be eliminated.
The UHMS HBO2 Safety Committee recommends that a proper risk assessment be performed by the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility, identifying the components of the Cook Doppler Wire and any potential for harm caused by the item itself (physically) or to the patient (medically) if they are disconnected from this diagnostic device while hyperbaric oxygen therapy is provided. If your risk assessment concludes that the wire can remain in place, we would recommend that mitigations be put in place to ensure that the Doppler Blood Flow Monitoring System is removed, and that the hyperbaric team identifies this during the pre-therapy safety stop, time-out, or pause.
The following observations from Safety Committee members may assist you in the decision-making process:
- One member has encountered several doppler wires of this type and after assessment has allowed them to remain in place in the Monoplace or Multiplace environment once they are disconnected from the doppler unit. Following multiple cycles, no damage to the ultrasound transducer assembly has been reported at this facility.
- Another member offered the following observations regarding the Cook-Swartz Doppler and use in a hyperbaric chamber, oxygen-filled and pressurized monoplace or air pressurized multiplace, commenting only on the non-medical aspects:
- I do not perceive an issue with the silicone cuff as it is internal and has no known gas pockets. Also, silicone is commonly utilized in hyperbaric oxygen environments.
- I do not perceive an issue with the retention tab, braided wire, or transducer assembly as these are similar to TCOM electrodes, and when disconnected, they are passive.
- The Doppler Blood Flow Monitoring System must be disconnected from the patient probe while the patient is inside the chamber.
- The Doppler Blood Flow Monitoring System is not permitted inside of the chamber.
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc. LINK
- National Fire Protection Agency (NFPA). (2021). “NFPA 99 2021 Edition: Health Care Facilities Code.” Quincy, Massachusetts. LINK
- Cook Medical. “Cook-Swartz Doppler Probe.” Website accessed on 3/17/21. LINK
- Undersea and Hyperbaric Medical Society. (2018). Clinical Hyperbaric Facility Accreditation Manual (4th ed.). North Palm Beach, FL: Undersea and Hyperbaric Medical Society, Inc. LINK, MANUAL
- Undersea and Hyperbaric Medical Society. (2014). Position Statement: Safety Time Out/Pause - "Stop". Undersea and Hyperbaric Medical Society, Inc. LINK
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Patient has nail powder gel that is 9 days old. Is it safe to put patient in chamber? Patient does not want to remove powder gel.
Posted 4/6/2021
Q:
Patient has nail powder gel that is 9 days old. Is it safe to put patient in chamber? Patient does not want to remove powder gel.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Medical Director and Safety Director of your facility.
The UHMS HBO2 Safety Committee applauds you for considering very carefully the risks of flammable vapors that are produced by these types of products. The vapor given off by the nail polish is mainly due to the acetone content. However, when the polish is fully dry, the risk from the vapor emission is greatly reduced. It is highly likely that the polish has been fully cured after nine days.
That being said, it is known that Powder Gel-type nail polish does not dry immediately on its own. In some cases, a UV light curing device is utilized immediately following the application. In this instance, the polish is almost immediately dry. Cure times for non-UV light polish is 10-20 minutes (see reference below).
We recommend that hyperbaric practices develop a standardized, written approach to nail polish and other cosmetics, and that this information be shared with patients during the consultation and education process. Many facilities will include information of this nature within a patient education guide or pamphlet. It may be helpful to apply a general rule, (such as: Wait 12, 18, or 24 hours after application). It is also known that some facilities will allow nail polish so long as it is completely dry (no residue) and has no residual smell. In any case, this standardized approach should be driven from a risk assessment conducted by the Hyperbaric Safety Director and Hyperbaric Medical Director of your facility.
We encourage you to resource the references listed below which may assist you in your decision making.
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- Barry, R. C. (2020). How to determine if a material is safe for use in the hyperbaric chamber. In W. T. Workman & J. S. Wood. (Eds.), Hyperbaric facility safety (2nd ed., pp. 355). Best Publishing Company.
- National Fire Protection Agency (NFPA). (2018). NFPA 99 2018 Edition: Health Care Facilities Code, Chapter 14 – Hyperbaric Facilities. Quincy, Massachusetts.
- News Article: “A fire hazard in your makeup bag,” Accessed 3/29/2021, LINK
- Undersea and Hyperbaric Medical Society, “MEDFAQ: Dressings, 10/23/2020,” Accessed 3/29/2021, LINK
- Web Source, “How to dry gel nail polish,” Accessed 3/29/2021, LINK
- Workman, W. T., & Wood, J. S. (2020). Hyperbaric Facility Safety: A Practical Guide (2nd ed.). Best Publishing Company.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is there any special considerations for treating patients that have a colostomy or ileostomy bag/pouch?
Posted: 4/6/2021
Q:
Is there any special considerations for treating patients that have a colostomy or ileostomy bag/pouch?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Medical Director and Safety Director of your facility.
Ostomy devices, or an ostomy pouching system is a prosthetic medical device that provides a means for the collection of waste from a surgically diverted biological system (colon, ileum, bladder) and the creation of a stoma. Pouching systems are most commonly associated with colostomies, ileostomies, and urostomies.
The UHMS HBO2 SC recommends the creation of procedural documents specific to your practice that will accommodate your hyperbaric setting. These documents should be designed in accordance with your hospital’s nursing or gastroenterology guidelines, and approved by the Hyperbaric Safety Director and Hyperbaric Medical Director of your facility.
When considering the treatment of a patient with one of these devices in a hyperbaric chamber, the chief concern should be the effect of pressure changes on the gas that may accumulate in the bag over the course of treatment. Additionally, it is recommended that the container is emptied prior to therapy to avoid overfilling. It may be helpful for your practice to review any steps that should be accomplished during the pre-therapy safety stop, time-out, or pause.
We recommend that the following steps be applied when providing hyperbaric oxygen therapy in the Multiplace chamber to a patient with a colostomy or ileostomy bag/pouch:
- Empty ostomy appliance and void any accumulated gas just prior to start of therapy.
- Void excess gas in ostomy appliance prior to depressurization.
We recommend that the following steps be applied when providing hyperbaric oxygen therapy in the Monoplace chamber to a patient with a colostomy or ileostomy bag/pouch:
- Empty the ostomy appliance and void any accumulated gas just prior to start of therapy.
- If physically and cognitively able to perform, instruct patient to void excess gas in ostomy appliance prior to depressurization.
- If the patient is unable to resolve this, the ostomy appliance may require voiding of excess gas immediately following patient removal from the monoplace chamber.
REFERENCES:
- Undersea and Hyperbaric Medical Society. (2018). Clinical Hyperbaric Facility Accreditation Manual (4th ed.). North Palm Beach, FL: Undersea and Hyperbaric Medical Society, Inc. LINK, MANUAL
- Undersea and Hyperbaric Medical Society. (2014). Position Statement: Safety Time Out/Pause - "Stop". Undersea and Hyperbaric Medical Society, Inc. LINK
- United Ostomy Associations of America. "Ostomy Information," Retrieved March 29th, 2021.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is it safe to treat a patient with HBO that has Calypso Beacon Transponders implanted. He has 3 transponders implanted near his prostate due to radiation treatments he received a few years back. The company responded with: ** 2021-06-07 08:50:00 - Product Web Request Request: Are there any precautions for a patient undergoing Hyperbaric Oxygen Therapy? Or Diving? From System Operators manual: No specified indications under compatibility, contraindications, warnings and precautions or operational safety ab
Posted: 7/7/21
Q:
Is it safe to treat a patient with HBO that has Calypso Beacon Transponders implanted? He has 3 transponders implanted near his prostate due to radiation treatments he received a few years back.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Medical Director and Safety Director of your facility.
The UHMS HBO2 Safety Committee recommends that a proper risk assessment be performed by the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility, identifying the potential for this item to cause harm to the patient if hyperbaric oxygen therapy is provided. Several members of the Committee have investigated this item, contacted the manufacturer, and identified several risk factors and other details for your consideration:
- These devices have not been tested under hyperbaric conditions by the manufacturer. Members of our committee have encouraged the company to examine the need for this further and have provided the contact information of a group that could accomplish this.
- The Calypso Beacon Transponder is constructed with a glass outer sheath that may rupture if exposed to increased atmospheric pressure. The contents of the device could then be exposed to the surrounding tissue. It is not known if the contents could be harmful to patients.
- The Calypso Beacon Transponder is subjected to gamma radiation during the production process to promote sterilization of the device.
- We did not discover a safety data sheet for this device, but a 510(k) premarket clearance was discovered. LINK
- If the patient were to require emergent hyperbaric oxygen therapy, it is the view of this committee that the therapy should not be delayed due to the presence of this item.
- The committee located several documents related to the Calypso Beacon Transponder that may aid you in the decision-making process. (See references below)
If your risk assessment of this device concludes that the potential for harm is low and the patient would benefit from therapy, we would recommend that the patient be well-informed, and your risk assessment is fully documented by the HMD and HSD of your facility. You may also want to consider informing and receiving input from the patient’s oncology team.
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc. LINK
- FDA 510(k) resource page, US Food and Drug Administration. Accessed July 2, 2021. LINK
- Toufik D, PhD., “Presentation: Multivendor SBRT/IGRT The Calypso 4D Localization and Tracking System / Elekta Synergy-S,” Practical Medical Physics Symposium, AAPM 54th Annual Meeting, 2012. LINK
- Varian Medical Systems, Instructions – “Beacon® Care Package for Prostate,” LINK
- Varian Medical Systems, Product Sheet – “CALYPSO SOFT TISSUE (17G) BEACON TRANSPONDER.” LINK
- Varian TPS Helpdesk, email responses from web inquiries - received 6/21/2021 and 6/22/2021.
Closure Summary: “Thank you for your patience, while I have been engaged in discussions with Product Management and Engineering.
The capsule of the transponder is air-tight and there is no liquid within.
The lung beacons were tested to 2 bar pressure. However, the design for the lung beacons (which has a plastic tube around the vial for holding the legs) is very different from the prostate beacons.
No pressure testing has been done for the prostate beacons.
Recreational divers frequently go to 100 ft depth (3 atm of pressure), and certainly hyperbaric oxygen chambers reach this sort of pressure Thus, I am afraid that the integrity of neither the lung nor the prostate beacon can withstand that.
In fact, since there is no pressure testing for the prostate beacons, so it is unknown when this could fail.
Regards,
Loretta
Loretta Lewandowski, Ph.D., D.A.B.R.
Medical Physicist, North America Clinical Help Desk
Varian Medical Systems
United States”
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
are there any issues with antibiotic beads and hyperbaric treatments. Pt had surgery to remove the osteo bone and beads were placed in wound and sutured closed. is pt safe to treat with HBO?
Posted: 8/2/21
Q:
Are there any issues with antibiotic beads and hyperbaric treatments. Pt had surgery to remove the osteo bone and beads were placed in wound and sutured closed. is pt safe to treat with HBO?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Medical Director and Safety Director of your facility.
The UHMS HBO2 Safety Committee believes there to be a low or zero risk to the patient from the mechanical effects of pressure changes on the antibiotic beads. Typically, these beads are dissolvable and therefore have a certain degree of solubility that should not be affected by surrounding pressure changes. The beads break down over time, facilitating new bone growth once the infection is gone.
Some antibiotic beads are made of polymethyl methacrylate (PMMA). This is the same material that is found in the acrylic hulls and windows of many monoplace and multiplace chambers. This type does not dissolve and will normally be removed in a week to ten days. In some cases, this material is even left inside of the body. We would recommend that you investigate which type of product is present so that all involved can remain well informed.
Mechanical risks aside, there is a theoretical risk for increased medicinal uptake of the product, and therefore a theoretical reduction in the overall length of antibiotic therapy due to increased absorption. However, several of our committee members have witnessed good patient outcomes with no adverse effects in several patients they have treated over many years with both types of antibiotic beads. To our knowledge, no research studies exist related to the absorption rate of these products in the hyperbaric setting.
REFERENCES:
DeCoster, T. A., & Bozorgnia, S. (2008). Antibiotic beads. JAAOS-Journal of the American Academy of Orthopaedic Surgeons, 16(11), 674-678.
McPherson, E., Dipane, M., & Sherif, S. (2013). Dissolvable antibiotic beads in treatment of periprosthetic joint infection and revision arthroplasty-the use of synthetic pure calcium sulfate (Stimulan®) impregnated with vancomycin & tobramycin. Reconstructive Review, 3(1).
Respectfully,
The UHMS HBO2 Safety Committee
any information on cardiac Watchman implant from Boston Scientific? Tried calling company but have not received call back. Safe for HBO?
Date: 3/11/2020
Q:
Any information on cardiac Watchman implant from Boston Scientific? Tried calling company but have not received call back. Safe for HBO?
A:
Thank you for your question. The UHMS HBO2 safety committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the medical director and safety director of your facility.
This device is similar in design and purpose to other types of cardiac stents. The particular difference is that this implant helps to reduce clotting in a specific region of the heart known as the left atrial appendage. Patients with atrial fibrillation may benefit from the use of this implant by reducing the risk of stroke due to clots that tend to form in this area of the heart.
Several members of the Safety Committee have indicated that there are no overt concerns raised that would prohibit a patient with a cardiac Watchman Implant from receiving Hyperbaric Oxygen Therapy. One of the committee members consulted Boston Scientific and spoke with their representatives. They confirmed that “There are no issues with the Watchman and HBO therapy”. Additionally, the committee consulted a cardiovascular specialist who is familiar with this implant, who agreed with this conclusion. Therefore the UHMS Safety Committee sees no reason to withhold hyperbaric oxygen therapy from a patient due to the presence of a cardiac Watchman implant.
Respectfully,
The UHMS Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is PET plastic permitted in hyperbaric chamber? We have used single water bottles but infection control would like us to switch to individual use disposable wo labels.
Posted: 9/27/2021
Updated: 2/7/2022
Q:
Is PET plastic permitted in hyperbaric chamber? We have used single water bottles but infection control would like us to switch to individual use disposable wo labels.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
Many of our committee members are familiar with this rather common practice (In 2018, a U.S. survey revealed that 35 of 37 Hyperbaric Facilities allow plastic water bottles in the chamber). With a few simple mitigations, this item should not pose any problems within the Monoplace or Multiplace hyperbaric environment. The material itself - Polyethylene Terephthalate (PET) is known to be flame retardant. According to sources referenced below, this material appears to melt at around 500°F. The UHMS HBO2 Safety Committee does not view this item to be a significant fire risk when combined with common patient grounding principles in place.
There are several considerations that you may wish to address before introducing the use of capped bottles. The mitigations you choose should be documented within your risk assessment, which should be completed by the Safety Director and signed by your Safety Director and Medical Director. For more guidance on performing a risk assessment, we encourage you to review NFPA 99, 14.3.1.6.4.3 (2021) annex notes on risk assessment and consider obtaining a copy of “Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities” (ref 1).
It is also important to note that before introducing a new item/process, clear communication is provided to staff and any training needs are addressed. You should also ensure that any new procedural steps appear on your pre-treatment checklist and are covered during your pre-treatment safety time out/stop/pause (per NFPA 99 (2021), 14.3.1.6.1.3).
You may consider the following mitigations as you complete your risk assessment:
- There is the potential for Boyle’s law to act upon trapped gases within the bottle during decompression. To address this, you may wish to leave the bottles uncapped, loose, or ventilate the bottles with a large-bore needle (at least 12 GA recommended).
- We are aware of at least one facility that leaves the bottles capped. They chose to use low-mass, environmentally friendly bottles (thinner walled bottles) that will fail at lower pressures. They have found that other, more robustly made bottles have a tighter thread engagement, providing a greater potential to injure patients if they fail.
- The Safety Committee does not endorse a particular style of drinkware. Rather, we would advise that you apply the safety principles described here to address the risk for your situation.
- We are aware of facilities who utilize sport bottle-style pop-tops rather than bottle caps.
- Consider the removal of paper labels (if present).
NOTE: Regarding the presence of residual glue resulting from the removal of labels, the UHMS HBO2 Safety Committee does not see this as a significant risk if no odor is present.
You may also wish to consider applying the following COVID-related mitigations:
- Use single-use only plastic bottles
- Clean the bottles with a surface disinfectant wipe and let air dry
- Using new gloves, break the cap seal and close gently prior to use
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc. LINK
- Chimiak, J. (2010). Evaluating Equipment and Materials for Use in a Hyperbaric Oxygen Environment: Clinical Hyperbaric Evaluation and Testing (CHET) Program. In: Hyperbaric Facility Safety: A Practical Guide (1st ed., 3rd reprint). Best Publishing Company. LINK
- National Fire Protection Association (NFPA). (2021). “NFPA 99 2021 Edition: Health Care Facilities Code.” Quincy, Massachusetts. LINK
- Pullis, M. (2019) “National Survey of Equipment Used in Hyperbaric Facilities,” UHMS ASM Pre-Course Presentation: Hyperbaric Oxygen Safety: Clinical and Technical Issues LINK
- Undersea and Hyperbaric Medical Society. (2018). Clinical Hyperbaric Facility Accreditation Manual (4th ed.). North Palm Beach, FL: Undersea and Hyperbaric Medical Society, Inc. LINK, MANUAL
- Undersea and Hyperbaric Medical Society. (2014). Position Statement: Safety Time Out/Pause - "Stop". Undersea and Hyperbaric Medical Society, Inc. LINK
- Web Reference: “PET – Density, Strength, Melting Point and Thermal Conductivity,” LINK, Accessed 9/3/2021
- Workman, W. T., & Wood, J. S. (2020). Hyperbaric Facility Safety: A Practical Guide (2nd ed.). Best Publishing Company. LINK
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
I have a question pertaining to the Clear Com Belt pack communication systems that are being used in multiplace chambers. When I first started in 2007 their belt back did not have an O2 marker on them. In the present facility that I work in they have units that have the O2 marker on them and some that don’t. I have tried to reach out to Clear-com and have not received a response. Can the non O2 marked units be used in the chamber if we use Nicad / NIHM batteries?
Posted: 9/24/2021
Q:
I have a question pertaining to the Clear Com Belt pack communication systems that are being used in multiplace chambers. When I first started in 2007 their belt back did not have an O2 marker on them. In the present facility that I work in they have units that have the O2 marker on them and some that don’t. I have tried to reach out to Clear-com and have not received a response. Can the non O2 marked units be used in the chamber if we use Nicad / NIHM batteries?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
Key factors to consider when evaluating equipment for the hyperbaric (multiplace – air) environment:
Communicating with the Manufacturer:
- Consider reaching out to the manufacturer to learn more about the device, especially if there are limited performance details/specifications in the OEM manual.
- Try to gain an understanding of what types of stress the device was subjected to during the manufacturing and testing phase.
- You may wish to make them aware of your intentions or you may remain anonymous.
- It should be noted that any modifications to the device or use other than as recommended by the manufacturer risks voiding any warranty on the product.
- If you discover that the non “O2” version has been tested previously under hyperbaric conditions, we suggest that this may be utilized as validation of your final assessment, but we do not recommend that this is the entirety of device approval. Simply put, we recommend a formal risk assessment regardless of testing methods.
- We strongly encourage that you seek assistance from your hospital biomedical engineering group and perhaps your hospital safety or legal teams. There are many useful examples of published risk assessment strategies applied to medical devices in the literature. Because communication devices may require the application of several safety mitigations, reviewing these strategies can provide useful guidance when considering the safety of battery-powered portable communication equipment in the multiplace (air) hyperbaric environment. There are several examples of medical device approval processes found in this MEDFAQ response.
- The National Fire Protection Association 99 Health Care Facilities Code, 2021 edition, chapter 14, lists the temperature, electrical limits, and responsibilities of the HSD regarding equipment used in Class A and B chambers. You should have this reference in your library.
- Considering the power source, we suggest ensuring that the battery remains secure within the housing and performing routine inspections. Consider involving a Biomedical Engineering representative for this process. Addressing the risk of the potential to generate heat, you should confirm the type of batteries contained within the beltpack. Along with the main battery power, the beltpack may also contain a low-power, non-rechargeable lithium battery, typically used to maintain a memory of system settings. (Disposable alkaline or silver oxide batteries are safe but are not always an option). Disposable lithium batteries are safer than rechargeable lithium battery types such as lithium-ion or lithium polymer, both of which can suffer runaway fires due to the electrolyte used in these products. Again, it is wise to involve a Biomedical Engineering representative in your risk assessment process.
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- National Fire Protection Agency (NFPA). (2021). NFPA 99 2021 Edition: Health Care Facilities Code. Quincy, Massachusetts. https://www.nfpa.org/
- Undersea and Hyperbaric Medical Society, MEDFAQ Response, “Telemetry Box in a multiplace chamber,” Accessed 9/24/2021, LINK
- Workman, W. T., & Wood, J. S. (2020). Hyperbaric Facility Safety: A Practical Guide (2nd ed.). Best Publishing Company.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Omnipod Dash for Hyperbaric use. Manufacturer says nothing about HBOT. This is what I found: The site warns that: The atmospheric pressure in an airplane cabin can change during flight, which may affect the Pod's insulin delivery. It also says Operating ATM 700hPA - 1060hPA. Powered by rechargeable Li-Ion 3.7V, 1300mAh.
Posted: 11/15/21
Q:
Omnipod Dash for Hyperbaric use. Manufacturer says nothing about HBOT. This is what I found: The site warns that: The atmospheric pressure in an airplane cabin can change during flight, which may affect the Pod\'s insulin delivery. It also says Operating ATM 700hPA - 1060hPA. Powered by rechargeable Li-Ion 3.7V, 1300mAh.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility. Whether you ultimately allow this item or not, we recommend that a thorough risk assessment be performed by the HSD in conjunction with the HMD when evaluating items of this type.
According to public information pertaining to this product, the Omnipod Dash system consists of “a pod which is worn on the body which carries and delivers insulin, plus a wireless Personal Diabetes Manager (PDM) connected to the pod that controls insulin delivery. The Omnipod has several differentiating features from conventional continuous subcutaneous insulin infusion (CSII) therapy including a tubeless waterproof pod and automated priming and cannula insertion. The Omnipod DASH system has a touchscreen PDM interface, Bluetooth wireless technology, and wireless internet connectivity.”
Pertaining to the Monoplace hyperbaric (NFPA Class B) environment, this device contains a battery which would prohibit its use in this setting. In the Multiplace (NFPA Class A) environment, there may be several risk factors that should be considered prior to allowing a device of this type. Chief among them should be, “Does the device present a fire hazard?” and, “Does the change in atmospheric pressure impact the devices’ ability to operate normally?”
Although not specifically prohibited by NFPA 99, chapter 14 (2021), we advise you to use caution when considering any battery in the multiplace hyperbaric environment and consider the item’s potential to fail or generate more heat than usual. Venting or purging the device with Air/Nitrogen may be considered. Working with the manufacturer and/or Biomedical Engineering teams in these cases is always recommended.
Additionally, the minimum and maximum tolerable pressures provided from the manufacturer relate to the following values:
Minimum: 700hPa (millibar) or 9878. 4 feet altitude which is approximately 73 kPa absolute
Maximum: 1060 hPa (millibar) or -1200 feet which is approximately 106 kPa absolute
Further testing is needed to confirm, but these values indicate that the device may not operate as designed when exposed to increased or decreased atmospheric pressure beyond these values.
One of our Committee members reached out to a local representative for the Omnipod Dash and returned the following information:
- It is not designed to give more than .05 units per dose
- It contains a SMA wire that heats up to deliver the dose
- The SMA wire is NiTinol (Nickel & Titanium)
- It has a magnetic field, so it is not MRI compatible
- If shorted, it will alarm and stop completely
Based upon the information reviewed, the UHMS HBO2 Safety Committee cannot recommend the use of this product in the hyperbaric environment unless it is confirmed that changes in atmospheric pressure do not affect the function of the device.
REFERENCES:
- Pillalamarri, S. S., Huyett, L. M., & Abdel-Malek, A. (2018). Novel bluetooth-enabled tubeless insulin pump: a user experience design approach for a connected digital diabetes management platform. Journal of diabetes science and technology, 12(6), 1132-1142. LINK
- Thompson, B., & Cook, C. B. (2019). Insulin pumping patches: emerging insulin delivery systems. Journal of diabetes science and technology, 13(1), 8-10. LINK
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
We are treating a patient who had a Zio XT ECG patch placed yesterday. I am unable to find any information on the patch and hyperbaric oxygen. The company is unable to provide me with any documentation of the safety of use in the hyperbaric environment. Do you know of anyone currently using the patch in the HBO(multiplace) environment?
Posted: 11/15/21
Q:
We are treating a patient who had a Zio XT ECG patch placed yesterday. I am unable to find any information on the patch and hyperbaric oxygen. The company is unable to provide me with any documentation of the safety of use in the hyperbaric environment. Do you know of anyone currently using the patch in the HBO (multiplace) environment?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
The UHMS HBO2 Safety Committee cannot endorse a specific device for use in the chamber. That said, we do not endorse the use of this device in a monoplace (Class B) chamber. We can provide you with specific resources that may assist you in your evaluation process for the multiplace (Class A) in an air-filled environment. Again, this is not an endorsement by the UHMS HBO2 Safety Committee for the use of this device in the Multiplace Hyperbaric Environment. Rather, we hope that you will consider these suggestions in your individual approach:
Key factors to consider when evaluating equipment for the hyperbaric (multiplace – air) environment:
- We strongly encourage a formal risk assessment of the device, with assistance from your hospital biomedical engineering group and perhaps your hospital safety or legal teams.
- If you discover that the device has been tested previously under hyperbaric conditions, we suggest that this may be utilized as validation of your final assessment, but we do not recommend that this is the entirety of device approval. Simply put, we recommend a formal risk assessment regardless of testing methods. (Exception: Modern ICD’s and Pacemakers are commonly tested by the manufacturer for function under pressure. Therefore, use under increased atmospheric conditions does not constitute an off-label use of those devices.)
- Consider reaching out to the manufacturer to learn more about the device, especially if there are limited performance details/specifications in the product manual.
- Try to gain an understanding of what types of stress the device was subjected to during the manufacturing and testing phase.
- You may wish to make the manufacturer aware of your intentions or you may remain anonymous.
- Regardless of the manufacturer’s response, there may be good reason for you to proceed with the evaluation, as this device would offer uninterrupted monitoring of the patient and may be vital to the continuum of care to the patient.
- It should be noted that any modifications to the device or use other than as recommended by the manufacturer risks voiding any warranty on the product.
- If evaluating a medical device, it is understood that few are intended to be used in the Multiplace hyperbaric environment. Therefore, consider that such use will likely fall into the FDA category of "Off-Label" and Investigational Use Of Marketed Drugs, Biologics, and Medical Devices “. You may also wish to review gov: Frequently Asked Questions about Medical Devices for more information.
- At least one major academic tertiary referral institution’s legal team with experience in medical device modification across its entire complex and constantly changing needs of subspecialty patient care including hyperbaric medicine interprets current FDA regulations in the following fashion.
“The program (modification and testing of medical devices for safe use in the hyperbaric environment) is not subject to FDA regulation. FDA regulates manufacturers and not the practice of medicine. Physicians are able to use FDA approved products other than under the labeled indications as long as the physician meets certain criteria. FDA’s statement on this off-label use is as follows:
“Good medical practice and the best interests of the patient require that physicians use legally available drugs, biologics and devices according to their best knowledge and judgment. If physicians use a product for an indication not in the approved labeling, they have the responsibility to be well informed about the product, to base its use on firm scientific rationale and on sound medical evidence, and to maintain records of the product's use and effects. Use of a marketed product in this manner when the intent is the "practice of medicine" does not require the submission of an Investigational New Drug Application (IND), Investigational Device Exemption (IDE) or review by an Institutional Review Board (IRB).”
- The National Fire Protection Association 99 Health Care Facilities Code, 2021 edition, chapter 14, lists the temperature, electrical limits, and responsibilities of the HSD regarding equipment used in Class A and B chambers. You should have this reference in your library.
- Regarding batteries, we suggest ensuring that batteries remain secure within the housing and receive routine inspections. Consider involving a Biomedical Engineering representative for this process. Disposable lithium batteries are safer than rechargeable lithium battery types such as lithium-ion or lithium polymer, both of which can suffer runaway fires due to the electrolyte used in these products. Again, it is wise to involve a Biomedical Engineering representative in your risk assessment process.
- Pay attention to any sealed air pockets within the housing that could be affected by Boyle’s Law. Ventilation of the housing may be necessary. For tracking purposes, you might consider labeling each device so that the care of those devices can be tightly controlled.
Key factors to consider when evaluating the Zio XT ECG patch for the hyperbaric (multiplace – air) environment:
- Using the device in an increased atmospheric environment is not in concert with the manufacturer’s environmental specifications (iRhythm Technologies, Inc. ZioXT Service Manual, Pg. 19, Environmental Specifications).
- This device utilizes two lithium manganese dioxide coin cells. If these are secured within the housing, coin-batteries like these are unlikely to cause any issues. Power consumption appears to be miniscule, and there are unlikely to be significant air pockets. That said, pressure testing the device prior to exposure with a patient is recommended.
- As always, check with the manufacturer prior to testing. Gaining their advice and cooperation is ideal.
- A safety committee member contacted iRhythm Technologies, inc. and spoke to a representative who was able to provide a Clinical Reference Manual along with the following information regarding the Zio XCT ECG:
- The patch is not sterile/sterilized during the manufacturing process
- The device may be removed and replaced, but multiple removals will cause the adhesive to be ineffective.
- The Product Manual states that the device should not be submerged in water (likely to protect internal circuitry).
Respectfully,
The UHMS HBO2 Safety Committee
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- Burman F, Sheffield R, Posey K. Decision process to assess medical equipment for hyperbaric use. Undersea Hyperb Med. 2009;36:137–44. PMID: 19462753.
- National Fire Protection Agency (NFPA). (2021). NFPA 99 2021 Edition: Health Care Facilities Code. Quincy, Massachusetts. https://www.nfpa.org/
- US Food and Drug Administration. (2014). “Off-label” and investigational use of marketed drugs, biologics, and medical devices: information sheet. Silver Spring, MD. LINK
- Workman, W. T., & Wood, J. S. (2020). Hyperbaric Facility Safety: A Practical Guide (2nd ed.). Best Publishing Company.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
We have an HBO candidate with a suprapubic catheter. The catheter has a silver tip for UTI prevention. Would this style of catheter be contraindicated in the HBO setting? Bard was contacted by one of our HBO nurses and they informed us that there was not testing on this catheter under hyperbaric conditions.
Posted: 1/12/22
Q:
We have an HBO candidate with a suprapubic catheter. The catheter has a silver tip for UTI prevention. Would this style of catheter be contraindicated in the HBO setting? Bard was contacted by one of our HBO nurses and they informed us that there was not testing on this catheter under hyperbaric conditions.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
The UHMS HBO2 Safety Committee does not have concern with this item in either the Monoplace or Multiplace Hyperbaric environments. We do recommend the following considerations prior to the start of therapy:
- Ensure that the catheter is patent.
- Check that the bulb is filled with sterile water per manufacturer’s instructions.
- Ensure that the line is free of entanglement.
- Check that the catheter bag/reservoir is emptied prior to therapy.
We would also encourage you to examine the relevant reference materials below. Thank you for your inquiry and we hope this will assist you in the safe delivery of hyperbaric oxygen therapy.
Respectfully,
The UHMS HBO2 Safety Committee
REFERENCES:
- BARD MEDICAL. “A Guide for Nurses - Bard® Comprehensive Care Management of Catheters and Collection Systems,” Bard Limited, Forest House, Tilgate Forest Business Park, Brighton Road, Crawley, West Sussex, RH11 9BP, UK https://media.bardmedical.com/media/1679/a-guide-for-nurses.pdf
- BARD MEDICAL. “BARDEX® I.C. Foley Catheter - Product Details,” webpage accessed 1/11/2022. https://www.bardcare.uk/clinicians/view-products/foley-catheters/bardex-ic-foley-catheter/
- MEDFAQ Response. “Special considerations for colostomy or ileostomy bag/pouch,” Published 4/6/2021. LINK
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
I have a patient with a trach with alot of secretions. Is there some way to have suction in a monoplace chamber and/or humidified air? Thank you.
Posted: 2/7/2022
Q:
I have a patient with a trach with a lot of secretions. Is there some way to have suction in a monoplace chamber and/or humidified air?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
The UHMS HBO2 Safety Committee is aware of several hyperbaric clinics who have required this setup. Before taking this on, we recommend that the patient’s ability to self-suction is assessed by the HBO physician, proper patient education is provided, and the operational staff is trained in the setup and operation of the vacuum system. It is imperative that the vacuum regulator be pre-set and not internally manipulated during therapy, as increased vacuum well above normal can be attained with the regulator open to full vacuum. Doing so could cause great harm to the patient. That said, the setup described below could accommodate your needs and could be applied to maintain vacuum-assisted closure (VAC) therapy during their hyperbaric treatment, should the patient require it.
It is also possible to offer additional humidity for tracheostomy patients receiving hyperbaric oxygen therapy in the monoplace chamber. This is commonly done with the use of a heat moisture exchanger (HME), although this humidifying filter will have to be removed if suctioning is necessary. Again, it is important that the patient is educated well and is comfortable performing these actions alone within the monoplace chamber.
For more information on these practices, the Committee encourages you to review the work published by our hyperbaric colleagues:
Monoplace Suction System:
Excerpt from Weaver et al - Monoplace chamber safety guidelines, page 39:
A suction system for the monoplace chamber has been developed (25). (Drager also offers a suction unit with their monoplace chamber.) An Ohmeda vacuum regulator and suction canister are mounted in the chamber hatch (Fig. 13). The vacuum hose that drives the regulator is passed out of the chamber via an i.v. pass-through (no. 041-600-500, Cobe) or via a specialized port because i.v. passthroughs are occasionally in high priority. The pressurized chamber provides the gradient of pressure necessary to operate the vacuum regulator. The regulator should NEVER he turned to "Full" but rather to the "Regulate" position. A screw serving as a stop will prevent turning the vacuum regulator to the "Full" position (Fig. 14). The degree of vacuum can be adjusted outside the chamber by carefully positioning the handle of the 3-way stopcock and reading the degree of vacuum from the regulator gauge. This system allows nasogastric, oral, wound, or pleural suction during HBO therapy. This system should not be used for endotracheal suction as there is a potential for complications (effects of auto-PEEP, reduced alveolar ventilation, or hypoxemia if inadvertently left on). Chest tubes should have a Heimlich valve or waterseal in place even with suction, in case the suction unit fails or is not turned to the "On" setting. Slow decompression rates in patients with chest tubes are recommended to allow adequate venting of any intrapleural gas that is present.
REFERENCES:
Neuman, T. S., & Thom, S. R. (2008). Physiology and Medicine of Hyperbaric Oxygen Therapy. Elsevier Health Sciences. Weaver LK - Technical Aspects, Chapter 2 – Monoplace Hyperbaric Chambers, pg. 30-31. LINK
Weaver LK. A functional suction apparatus within the monoplace hyperbaric chamber. J Hyperbaric Med 1988; 3:165-171. LINK
Weaver, L., & Strauss, M. B. (1997). Monoplace hyperbaric chamber safety guidelines. Bethesda, MD: Undersea and Hyperbaric Medical Society (UHMS). LINK
Raleigh, G. W., Niezgoda, J. A., & Fabus, S. V. (2002). A VACUUM REGULATION SYSTEM FOR CONTINUING VACUUM ASSISTED CLOSURE THERAPY (VAC) IN MULTIPLACE AND MONOPLACE HYPERBARIC OXYGEN CHAMBERS. LINK
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
We have a patient with dentures that are firmly secured in place with denture glue, and they are refusing to remove them for treatment. Can we allow dentures and over-the-counter bonding compounds like Sea-Bond©, Poligrip©, or Fixodent© in the Monoplace / Multiplace chamber?
Posted: 4/20/22
Q:
We have a patient with dentures that are firmly secured in place with denture glue, and they are refusing to remove them for treatment. Can we allow dentures and over-the-counter bonding compounds like Sea-Bond©, Poligrip©, or Fixodent© in the Monoplace / Multiplace chamber?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
The UHMS Safety Committee agrees that removing loose dentures prior to hyperbaric therapy is a good practice. However, we do not think it is unreasonable to leave secured dentures in place. As part of your local approval process, we would recommend that the HSD should identify all known risk factors and document any potential risk mitigations (Ref 1). It is well known that many facilities will remove “loose” dentures due to the increased risk of a blocked airway in the event of a seizure. In many cases, dentures are not easily removed. If used as directed, the bonding products on the market today will hold dentures firmly in place.
The UHMS Safety Committee would advise you to consider, at minimum, the following risk factors when completing your assessment:
Ingredients within the bonding agents/compounds:
- The bonding agents are made of several compounds that could, in theory, lead to an increase in the risk of flammable vapors. We are not aware of any published reports on this topic and we believe the impact on vapor load is nominal. Mitigating factors may be:
- There is a limited volume of glue present.
- The bonding compound is not fresh and has largely off-gassed by the time that treatments take place
- The moist environment of the mouth will greatly decrease the potential for ignition.
- You may wish to contact the manufacturer or retain SDS information as you perform your risk assessment.
Risk of a patient choking on loose dentures in the event of a seizure:
- As described above, many bonding products on the market today will hold dentures firmly in place for many hours.
- Consider adding a pre-therapy question related to dentures during intake screening.
- Consider inquiring of the patient how firmly the dentures are in place (i.e., they are clattering, easily moved with the tongue, or obviously loose). If they are easily removed, this may be the safest option.
- Consider that keeping dentures in place is likely to be helpful for emergency response teams by maintaining a more secure airway during resuscitation efforts (Ref. 2).
Communication considerations:
- Removing dentures may make it more difficult for the patient to enunciate
- Communication is a key factor in treating hyperbaric patients. Consider keeping secure dentures in place to avoid this barrier.
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc. LINK
- Conlon, N. P., Sullivan, R. P., Herbison, P. G., Zacharias, M., & Buggy, D. J. (2007). The effect of leaving dentures in place on bag-mask ventilation at induction of general anesthesia. Anesthesia & Analgesia, 105(2), 370-373. LINK
BIBLIOGRAPHY:
- National Fire Protection Agency (NFPA). (2021). “NFPA 99 2021 Edition: Health Care Facilities Code.” Quincy, Massachusetts. LINK
- Safety Committee MEDFAQ Response: “Hair Weave or extension with Keratin Glue,” Published 10/2015. LINK
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
I have a patient that has a Braun ezpump for antibiotics infusing into a picc line. It infuses 10ml/hr. Could this pump go into the chamber?
Posted: 5/20/22
Q:
I have a patient that has a Braun ezpump for antibiotics infusing into a picc line. It infuses 10ml/hr. Could this pump go into the chamber?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
Several elastomeric-style pumps have been tested within a hyperbaric environment. However, the UHMS HBO2 Safety Committee is not aware of any performance testing of the Braun Easypump™ Elastomeric Infusion Pump inside of a hyperbaric chamber. We would encourage you to first determine the necessity of the item for the time duration required to complete the therapy. Oftentimes, antibiotics may be delayed or briefly interrupted without negative outcomes. If it is possible and safe to delay either the HBO Therapy or the infusion, we would recommend this approach.
It is important to note that changes in delivery rate have been noticed during air travel in another make and model (Baxter Infusor pump). It is plausible then that changes to the delivery rate of the Braun Easypump™ may also be effected under hyperbaric conditions. However, it is noted that other elastomeric pumps have been tested and shown to function well under hyperbaric conditions. For example, the On-Q elastomeric pain pump has been tested under hyperbaric conditions and demonstrated “no clinically significant change in the function of the On-Q infusion device during hyperbaric exposure for the usual clinical durations and hyperbaric pressures.”
If you are considering the option to test this device for safe use within the hyperbaric environment, we can provide you with specific resources that may assist you in your evaluation process. This information not an
endorsement by the UHMS HBO2 Safety Committee for the use of this device in the hyperbaric environment. Rather, we hope that you will consider these suggestions in your individual approach:
- We strongly encourage a formal risk assessment of the device, with assistance from your hospital biomedical engineering group and perhaps your hospital safety or legal teams.
- If you discover that the device has been tested previously under hyperbaric conditions, we suggest that this may be utilized as validation of your final assessment, but we do not recommend that this is the entirety of device approval. Simply put, we recommend a formal risk assessment regardless of testing methods. (Exception: Modern ICD’s and Pacemakers are commonly tested by the manufacturer for function under pressure. Therefore, use under increased atmospheric conditions does not constitute an off-label use of those devices.)
- Consider reaching out to the manufacturer to learn more about the device, especially if there are limited performance details/specifications in the product manual.
- Try to gain an understanding of what types of stress the device was subjected to during the manufacturing and testing phase.
- You may wish to make the manufacturer aware of your intentions or you may remain anonymous.
- Regardless of the manufacturer’s response, there may be good reason for you to proceed with the evaluation, as this device may be vital to the continuum of care to the patient.
- It should be noted that any modifications to the device or use other than as recommended by the manufacturer risks voiding any warranty on the product.
- If evaluating a medical device, it is understood that few are intended to be used in the Multiplace hyperbaric environment. Therefore, consider that such use will likely fall into the FDA category of "Off-Label" and Investigational Use Of Marketed Drugs, Biologics, and Medical Devices “. You may also wish to review FDA.gov: Frequently Asked Questions about Medical Devices for more information.
NOTE: Regarding medical device evaluation, at least one major academic institution’s legal team with experience in medical device modification has approached the current FDA regulations in the following fashion:
“The program (modification and testing of medical devices for safe use in the hyperbaric environment) is not subject to FDA regulation. FDA regulates manufacturers and not the practice of medicine. Physicians are able to use FDA approved products other than under the labeled indications as long as the physician meets certain criteria. FDA’s statement on this off-label use is as follows:
“Good medical practice and the best interests of the patient require that physicians use legally available drugs, biologics and devices according to their best knowledge and judgment. If physicians use a product for an indication not in the approved labeling, they have the responsibility to be well informed about the product, to base its use on firm scientific rationale and on sound medical evidence, and to maintain records of the product's use and effects. Use of a marketed product in this manner when the intent is the "practice of medicine" does not require the submission of an Investigational New Drug Application (IND), Investigational Device Exemption (IDE) or review by an Institutional Review Board (IRB).”
REFERENCES:
Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
Burman F, Sheffield R, Posey K. Decision process to assess medical equipment for hyperbaric use. Undersea Hyperb Med. 2009;36:137–44. PMID: 19462753.
Dohgomori, H., Arikawa, K., Gushiken, T., & Kanmura, Y. (2002). Accuracy of portable infusers under hyperbaric oxygenation conditions. Anaesthesia and intensive care, 30(1), 25-28.
Millar, I. L. (2015). Hyperbaric intensive care technology and equipment. Diving Hyperb Med, 45(1), 50-56.
National Fire Protection Agency (NFPA). (2021). NFPA 99 2021 Edition: Health Care Facilities Code. Quincy, Massachusetts. https://www.nfpa.org/
Perks, S., Blake, D. F., Young, D. A., Hardman, J., Brown, L. H., Lewis, I., & Pain, T. (2017). An assessment of the performance of the Baxter elastomeric (LV10) Infusor™ pump under hyperbaric conditions. Diving and Hyperbaric Medicine, 47(1), 33.
Salman, D., Barton, S., & Nabhani-Gebara, S. (2013). Effect of environmental conditions on performance of elastomeric pumps. American Journal of Health-System Pharmacy, 70(13), 1100-1100.
Tobias, J. D., Johnson, G. A., & Patel, M. (2011). Performance of the On-Q pain infusion device during hyperbaric therapy. Anesthesia & Analgesia, 113(2), 275-277.
US Food and Drug Administration. (2014). “Off-label” and investigational use of marketed drugs, biologics, and medical devices: information sheet. Silver Spring, MD. LINK
Wang, J. (2013). Effect of environmental conditions on performance of elastomeric pumps--author's reply. American Journal of Health-system Pharmacy: AJHP, 70(13), 1100-1101.
Workman, W. T., & Wood, J. S. (2020). Hyperbaric Facility Safety: A Practical Guide (2nd ed.). Best Publishing Company.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
We have a patient with the Medtronic Activa SC model 37603 brain stimulator (seizure disorder). The company states it is okay to 2ATA. Has anyone treated someone with such a device? (Monoplace
Posted: 6/14/2022
Q:
We have a patient with the Medtronic Activa SC model 37603 brain stimulator (seizure disorder). The company states it is okay to 2ATA. Has anyone treated someone with such a device? (Monoplace)
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
First of all, the Safety Committee appreciates your willingness to learn as much as you can about these devices and the potential risk they may add to the patient in your care. As with any medical device, a risk assessment performed by your HSD in conjunction with your HMD should be your first step. In this instance, the manufacturer has given parameters, and the HBO2 SC would advise that you would follow their recommendations.
In response to your specific inquiry of the committee with this device, none of our members have had experience treating a patient with a Medtronic Activa SC model 37603 brain stimulator. One member from Europe has shared his experience. Several other members have shared that they have treated patients with several different makes and models of stimulators made to stimulate the central nervous system. I will include some of their comments below. We have also included links to several resources in the references section that may help you conduct a risk assessment.
- I have not personally treated a patient with a deep brain stimulator; however, I know of patients that have been treated without issue.
- I have no experience with the Medtronic brain stimulator. We’ve treated with the Medtronic spinal stimulator previously – also limited to 2.0 ATA – without apparent adverse effect.
- We have treated some patients with those devices, and I know from our previous survey that some other hyperbaric facilities in Europe had done it as well. This includes also hyperbaric facility at the Karolinska Institute in Sweden. In my opinion:
- First, internal electrodes do not present any additional hazard in the hyperbaric environment
- Second, controlling device is quite similar to Implantable Cardiac Pacemakers (ICD) which means that they are all exposed to initial “unintentional” hyperbaric environment during the ISO-compatible ETO-standard sterilization process, when the pressure is from 1.7 up to 2.5 ATA (7–15 msw).
- Third, Medtronic stated about the compatibility of their ICD to hyperbaric pressure, but - as far as I am aware - not with IBS. Therefore, patients in our center are informed about the POSSIBLE INCREASED RISK for malfunction of the device, but it does not stop us in using HBOT (up to 2.5 ATA until now) both for chronic and emergency indications.
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- Burman F, Sheffield R, Posey K. Decision process to assess medical equipment for hyperbaric use. Undersea Hyperb Med. 2009;36:137–44. PMID: 19462753.
- Jagadeeswaran, I., & Chandran, S. (2022). ISO 11135: Sterilization of Health-Care Products—Ethylene Oxide, Requirements for Development, Validation and Routine Control of a Sterilization Process for Medical Devices. In Medical Device Guidelines and Regulations Handbook (pp. 145-153). Springer, Cham. LINK
- Medtronic, inc. (Updated March 2022). INDICATIONS, SAFETY, AND WARNINGS - Deep Brain Stimulation Therapy. Accessed 5/31/2022 LINK
- U.S. Food and Drug Administration (2022). Deep Brain Stimulator - Patient Manual. Accessed 5/31/2022 LINK
- Workman, W. T., & Wood, J. S. (2020). Hyperbaric Facility Safety: A Practical Guide (2nd ed.). Best Publishing Company.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Recently, an brain abscess patient with halo ring fixator was referred to our center. After vertified with case physician, the halo ring fixator was made of mainly plastic & carbon fiber with titanium pin. We are aware that titanium may pose an increased fire risk. Does UHMS committee have any suggestions to make the treatment safer? Is it necessary to cover the titanium pin with wet graze? Our chamber is a multiplace chamber which the patient will be given O2 via tracheostomy tube. Thanks.
Posted: 6/29/22
Q:
Recently, an brain abscess patient with halo ring fixator was referred to our center. After vertified with case physician, the halo ring fixator was made of mainly plastic & carbon fiber with titanium pin. We are aware that titanium may pose an increased fire risk. Does UHMS committee have any suggestions to make the treatment safer? Is it necessary to cover the titanium pin with wet graze? Our chamber is a multiplace chamber which the patient will be given O2 via tracheostomy tube. Thanks.
A:
My name is Andrew Melnyczenko, Chair of the UHMS Hyperbaric Oxygen Therapy Safety Committee, and your question regarding allowance a fixator containing titanium in the multiplace environment was forward to me by John Peters, Executive Director of the UHMS.
Ultimately, the decision to allow any item into the hyperbaric environment is the joint responsibility of the Hyperbaric Safety Director and Medical Director of your facility. I will provide you with information to assist you in answering your question. You may consider that the testing performed on titanium that is often quoted in these instances was done in 100% oxygen environment, and under greater-than-clinical levels of pressure (4.4 ATA). Based upon the description in your question, it seems that your conditions do not meet those identified in this article. For this reason, and the improbability that these materials would need to be stressed to the point of breaking, the risk of fire should be low in the multiplace environment with oxygen monitoring and ventilation present to keep oxygen levels below 23.5%. I am aware of many instances where fixation devices such as the one you describe have been allowed inside multiplace chambers in an air environment, with oxygen monitoring and ventilation present to keep oxygen levels below 23.5%.
The 2021 NFPA 99 Health Care Facilities Handbook, 14.3.2.5* prohibits equipment made from cerium, magnesium and magnesium alloys in the Class A hyperbaric chamber. There is concern expressed within the handbook annex, A.14.3.2.2 regarding the potential risk of many products. Iron alloys, aluminum, human skin, plastic tubing etc may not self-extinguishing in an oxygen-enriched environment. Titanium and Titanium alloys are not specifically prohibited in the hyperbaric chamber by NFPA 99.
I will also refer you to several questions previously answered by the committee on the subject of titanium. These are publicly available on the UHMS MEDFAQ page:
https://www.uhms.org/resources/medfaqs-frequently-asked-questions-faq/safety-technical/162-item-approval.html?faq=36
https://www.uhms.org/resources/medfaqs-frequently-asked-questions-faq/safety-technical/162-item-approval.html?faq=137
I hope this information is beneficial. Thank you for reaching out to the UHMS Safety Committee.
Sincerely,
Andrew R. Melnyczenko
UHMS Safety Committee Chair
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Are there any suspected risks involved with the use of Invisalign (orthodontic product) during hyperbaric oxygen treatment in a multi-place chamber?
Posted: 7/6/2022
Q:
Are there any suspected risks involved with the use of Invisalign (orthodontic product) during hyperbaric oxygen treatment in a multi-place chamber?
A:
We see no concerns (UHMS SC Chair), but of course removing the retainer during treatment is recommended as there could be some trapped gas causing a “squeeze” which could occur during pressurization making the retainer more difficult to remove as well.
We have a patient with bilateral K Pro 1 lenses, can they go in the mono-place chamber or do they need to be removed prior to treatment. Are there any specific modifications needed for treatment?
Posted: 8/12/22
Q:
We have a patient with bilateral K Pro 1 lenses, can they go in the mono-place chamber or do they need to be removed prior to treatment. Are there any specific modifications needed for treatment?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
Before we respond to this question, it is important for our readers to understand this optical device a bit more. The Safety Committee would like to provide general information on the K-Pro Type 1 and Type II implants and procedure, taken from this article(7):
The Boston Type I Keratoprosthesis (BI-KPro) is an artificial cornea device. It is implanted as a treatment for many severe, recalcitrant corneal disorders that are not amenable to traditional corneal transplantation such as penetrating keratoplasty (PK). Although the device was initially rejected by ophthalmologists because of its high rate of complications, modifications to the mechanical design, as well as the development of antibiotic prophylaxis regimens and large-diameter bandage contact lenses, have allowed the BI-KPro to become a viable option for preserving or restoring vision.
The BI-KPro was first developed by Claes H. Dohlman, MD, PhD, at the Massachusetts Eye and Ear Infirmary in the 1960s, but it was not approved by the U.S. Food and Drug Administration until 1992. Since its approval, the BI-KPro has become more widely adopted in the United States and globally and is now considered a standard of care for the treatment of many otherwise blinding corneal diseases.
The Boston KPro is available in 2 variants, Type I and Type II, both of which contain an optic, as well as a front plate and a back plate, between which a donor corneal graft is placed. Type I is much more commonly used, as its implantation procedure more closely resembles PK surgery. It is available in both adult and pediatric sizes.
The UHMS HBO2 Safety Committee was unable to receive feedback from the manufacturer regarding the risk to patients with this implant receiving hyperbaric oxygen therapy. We suggest that this is a local decision and recommend that a risk assessment weighing the benefit of hyperbaric medicine versus the medical risk to the patient is performed(1). It this case, the primary responsibility rests upon the HMD of the hyperbaric clinic with input from the HSD and the patient’s Ophthalmology team. Members of the UHMS HBO2 Safety Committee have reached out to diving and ophthalmology physicians to inquire about this implant and the implant procedure. Their assessment revealed several points of consideration:
- These implants are not typically or easily removed.
- There are no obvious air spaces that would incur a mechanical hazard.
- Consultation between the Hyperbaric Provider and the Ophthalmology team who performed the procedure is recommended. A specific point that should be addressed by the patient's ophthalmologist is whether there are any gas bubbles in the eye. Intraocular gas bubbles are an absolute contraindication to both HBO2 therapy and diving.
- You may wish to consider delaying the therapy several weeks if this procedure occurred recently.
We will provide several resources(2,3,4,5,6) intended to guide you in the decision-making process. Thank you for reaching out to the UHMS HBO2 Safety Committee.
Respectfully,
The UHMS HBO2 Safety Committee
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- Butler Jr, F. K. (1995). Diving and hyperbaric ophthalmology. Survey of ophthalmology, 39(5), 347-366. LINK
- McMonnies CW, “Hyperbaric oxygen therapy and the possibility of ocular complications or contraindications” Journal of clinical and experimental optometry, 2015, Volume 98, Issue 2, Pages 122-125. LINK
- Simon, D. R., & Bradley, M. E. (1978). Corneal edema in divers wearing hard contact lenses. American journal of ophthalmology, 85(4), 462-464. LINK
- Simon, D. R., & Bradley, M. E. (1980). Adverse effects of contact lens wear during decompression. JAMA, 244(11), 1213-1214. LINK
- Socks, J. F., Molinari, J. F., & Rowey, J. L. (1987). Rigid gas permeable contact lenses in hyperbaric environments. NAVAL SUBMARINE MEDICAL RESEARCH LAB GROTON CT. LINK
- Starr, C. E., Klufas, M. A., Feldman, B. H., Bunya, V. Y., & Moon, C. Boston Keratoprosthesis (KPro). eWiki (aao.org), Accessed 6/20/22 LINK
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Hello, we have a patient status post radiation therapy and bilateral mastectomy. She currently has Natrelle silicone implants and our department is curious to see if you have any previous studies on HBO therapy on a patient with such implants. We contacted the manufacturer (Abbvie) and they state "No relevant information was identified". Thank you for your assistance.
Posted: 10/14/22
Q:
Hello, we have a patient status post radiation therapy and bilateral mastectomy. She currently has Natrelle silicone implants, and our department is curious to see if you have any previous studies on HBO therapy on a patient with such implants. We contacted the manufacturer (Abbvie), and they state: "No relevant information was identified". Thank you for your assistance.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
The UHMS HBO2 Safety Committee is aware of many centers who have successfully delivered hyperbaric therapy to patients with fluid-filled and silicone-filled implants. Many, if not most hyperbaric programs no longer screen for these items. The rationale behind this conclusion is that fluid-filled, sealed objects are largely incompressible (Described in: Fluid Mechanics Fundamentals and Applications, 2013). Many of our committee members report years of repeated exposures to varying depths of pressure, both in patients and inside attendants.
However, the UHMS HBO2 Safety Committee is aware of a study (Grippaudo, 2002) regarding implant conformational changes after exposure to pressure with an implant containing a cohesive gel filling. It is our understanding is that newer generation implants are more likely to have this cohesive gel filling. There is potential that asymmetric pressure applied to these devices from capsular contractions may also cause rupture of an older device that is significantly weakened. This may cause cosmetic issues. You may wish to discuss this potential during the informed consent process.
Grippaudo (2002) – subjected breast implants to 40 simulated recreational dives. The goal was to determine if implants exposed to elevated pressure results in structural or conformational changes. Dive profiles were to 39m twice daily with an 8-hour surface interval between dives for a total of 20 days. Staged decompression was carried out in accordance with US Navy tables. Implants were inspected for integrity and CT scans were performed after all dives were completed. No shell ruptures were noted and no changes in volume were noted; however, conformational changes were noted in the cohesive gel implants with distortion remaining after 12 months.
There are several other comments provided by Committee members that may be of interest to you in determining your approach to these items:
- In a separate study, testing of a variety of FDA silicones used in implants for use in hydraulic systems within manned atmospheres have shown that these fluids load and offload gases slower than humans and are not chemically altered when exposed to pure oxygen. They are not an issue in HBO clinical operations from a gas exchange standpoint. (No source available)
- It is reported that pressure tolerance testing at Duke University was conducted on silicone-filled implants approximately 15-20 years ago. Pressure did not appear to damage the implants. (No source available)
- With regards to diving, the general recommendation we give is to allow some time after the surgery for the body to properly encapsulate the implants, as some BCD straps might put some lateral pressure at the site.
- We receive many questions related to tissue expanders. We have not noticed any issues with saline or silicone-based expanders as they generally will not be subject to Boyle’s Law. Theoretically, a patient might feel a little pressure on the site during compression, but I cannot say that a patient ever actually reported that symptom.
- One committee member reports having the Abbvie Natrelle silicone implants and has been an inside attendant many times without issue.
- As long as a bubble is not present, there would be no concern. It is improbable that patients would feel anything untoward during compression or decompression. Regarding tissue expanders, these are incrementally filled with normal saline. It is theoretically possible to have a bubble collection in these devices since more fluid is incrementally added by injection. However, I do not recall ever having a problem with HBOT even here.
REFERENCES:
- Cengel, Y., & Cimbala, J. (2013). EBOOK: Fluid Mechanics Fundamentals and Applications (SI units). Chapter 2, pg. 44-46. McGraw Hill.
- Divers Alert Network, ”Breast Implants and Diving”. (Accessed 10/10/2022)
- Grippaudo, F. R., Minasi, P., Muratori, L., Rocco, M., Bruno, A., & Saracca, E. (2002). Mammary implants: laboratory simulation of recreational diving conditions. British journal of plastic surgery, 55(2), 120-123.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Would it it be possible to email me a copy of the list of the Go / no-Go list of items for HBOT? Or is this an item that needs to be purchased? Would you please let me know? Thank you in advance.
Posted: 12/12/2022
Q:
Would it it be possible to email me a copy of the list of the Go / no-Go list of items for HBOT? Or is this an item that needs to be purchased? Would you please let me know? Thank you in advance.
A:
My name is Andrew Melnyczenko, Chair of the UHMS HBO2 Safety Committee. Your question was recently forwarded to me by the Executive Director of the UHMS, Mr. John Peters. The committee would be glad to assist you in answering your question, but please realize that the ultimate responsibility for these types of questions rests with the hyperbaric Medical Director and Safety Director of the associated hyperbaric facility.
As you may be aware, Go/No-Go lists are not universal. They will vary by chamber type and the scope of the facility. These lists are always subject to the risk assessments and decisions made by the local Safety Director and Medical Director of the hyperbaric program. The provision of such a list is not the duty of the UHMS HBO2 Safety Committee, as we cannot dictate the policy and practice of a hyperbaric program. However, the UHMS HBO2 Safety Committee has certainly provided an opinion on many different items in response to various MEDFAQ inquiries. MEDFAQs is a place where common questions related to hyperbaric oxygen therapy are submitted, reviewed by the appropriate UHMS committee, and posted as a benefit to the hyperbaric community.
It is important to note that the safety committee will always steer these responses toward the individual responsibility of the program’s Medical and Safety Director. We lean heavily on the process of risk evaluation and determination of the need for risk mitigation. This pattern is duplicated over and over again in many of our responses.
Perhaps the best examples of this are found within the following links:
- https://www.uhms.org/resources/medfaqs-frequently-asked-questions-faq/safety-technical/162-item-approval.html?faq=467
- https://www.uhms.org/resources/medfaqs-frequently-asked-questions-faq/safety-technical/162-item-approval.html?faq=381
- https://www.uhms.org/resources/medfaqs-frequently-asked-questions-faq/safety-technical/162-item-approval.html?faq=194
- https://www.uhms.org/resources/medfaqs-frequently-asked-questions-faq/safety-technical/162-item-approval.html?faq=143
- (2021) NFPA 99, Chapter 14, Appendix A, A.14.3.1.6.4.3.
We hope that the information provided will assist you in answering your question. Please inform us if you have a more specific question about a particular item or topic. Thank you for reaching out to the UHMS and the UHMS HBO2 Safety Committee.
Sincerely,
Andrew Melnyczenko, BSHCA, CHT
Technical and Safety Director – Hyperbaric and Altitude Medicine, Division of Public Health, Infectious Diseases, and Occupational Medicine
Personal: (586) 612-3967
Office: (507) 538-5633
Pager: 127-00651
E-mail: melnyczenko.andrew@mayo.edu
Mayo Clinic
200 First Street SW
Rochester, MN 55905
mayoclinic.org
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
We have a patient with a failed flap. The patient presented today with dimethyl sulfoxide gel applied to the skin. Does this gel pose any risk to being in the chamber? Dimethyl Sulfoxide is a highly polar organic liquid that is used widely as a chemical solvent and a free radical scavenger. It shows a range of pharmacological activity including analgesia and anti-inflammation. Because of its ability to penetrate biological membranes, it is used as a vehicle for topical application of pharmaceuticals. Dime
Posted 1/6/2023
Q:
We have a patient with a failed flap. The patient presented today with dimethyl sulfoxide gel applied to the skin. Does this gel pose any risk to being in the chamber? Dimethyl Sulfoxide is a highly polar organic liquid that is used widely as a chemical solvent and a free radical scavenger. It shows a range of pharmacological activity including analgesia and anti-inflammation. Because of its ability to penetrate biological membranes, it is used as a vehicle for topical application of pharmaceuticals. Dimethyl sulfoxide appears as a clear liquid, essentially odorless. Closed cup flash point 192 °F. Vapors are heavier than air. Contact with the skin may cause stinging and burning and lead to an odor of garlic on the breath. An excellent solvent that can transport toxic solutes through the skin. High vapor concentrations may cause headache, dizziness, and sedation.
A:
The UHMS HBO2 Safety Committee can provide guidance to assist your decision making the but cannot endorse a specific product for use. The ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility. We recommend that a proper risk assessment be performed by the HMD and HSD; with careful consideration given to the flammability, NFPA 704 rating of the material, amount, potential for vapor release, chamber volume, and the fuel load added to the environment.
In our review, we have found that Dimethyl Sulfoxide Gel (commonly known as DMSO) does appear to have some highly exothermic reactions to certain materials, and as you rightly point out, this product is classified as a flammable solvent. While ignition sources can be controlled in the monoplace hyperbaric setting, there is concern that the gel compound will produce vapors that could potentially ignite in the presence of oxygen under increased atmospheric pressure. In addition, this product would produce highly toxic products from combustion. The SDS clearly states that the product “May form flammable/explosive vapor-air mixture.”
You may also wish to consider the increased medical-legal risk to the patient and perhaps the care team involving the use of veterinary products that are not evaluated by the FDA for human use. The surgeon’s instructions for use that you shared with us indicate that this product should be reapplied every 2-3 hours, so there may be a window to remove the ointment during hyperbaric therapy.
REFERENCES:
- Gaylord Chemical Company, L.L.C., “DMSO Health & Safety,” Accessed 12/21/2022 LINK
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- National Fire Protection Agency (NFPA). (2021). NFPA 99 2021 Edition: Health Care Facilities Code. Quincy, Massachusetts.
- SANCO Industries, Inc., “Safety Data Sheet: DMSO Gel,” Accessed 12/21/2022 LINK
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
What is current evidence based recommendation regarding patients wearing soft contact lenses during HBOT?
Posted: 3/24/2023
Q
What is current evidence-based recommendation regarding patients wearing soft contact lenses during HBOT?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
Gas-permeable contact lenses, both soft and hard styles, will not pose a risk for air trapping under the lens. There have been reports of hard contacts popping out of the eye or causing corneal edema, but these reports are decades old. Literature searches reveal no reports of issues with soft or hard contact lenses in the last 35 years.
Amongst our committee, we are not aware of any facilities that do not allow patients and inside attendants to wear soft and hard contact lenses in the chamber. We can report many years of successful diving, both in-water and in-chambers, without any complications.
REFERENCES:
- Butler Jr, F. K. (1995). Diving and hyperbaric ophthalmology. Survey of ophthalmology, 39(5), 347-366.
- Polse, K. A., & Mandell, R. B. (1971). Hyperbaric oxygen effect on corneal edema caused by a contact lens. Optometry and Vision Science, 48(3), 197-200.
- Simon, D. R., & Bradley, M. E. (1980). Adverse effects of contact lens wear during decompression. JAMA, 244(11), 1213-1214.
- Socks, J. F., Molinari, J. F., & Rowey, J. L. (1988). Rigid gas permeable contact lenses in hyperbaric environments. Optometry and Vision Science, 65(12), 942-945.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Can a home infusion system (ie. "hand grenade") be used in a monoplace chamber? Patient has implanted port.
Posted: 2/227/2023 Q:Can a home infusion system be used in a monoplace chamber? Patient has implanted port. A:Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility. Discovery Upon further review, the device your patient has is an elastomeric pump – an AVANOS C-Series (C100020) Homepump. Upon reaching out to the manufacturer, it was discovered that the company tested a device of the same design many years ago (On-Q Pain infusion device). AVANOS identified that the design of the flow restrictor has not changed. The testing suggested that that the pump would behave as designed while under hyperbaric conditions. Regardless of this finding, the Safety Committee recommends that your Medical Director and Safety Director assess the safety of this device for your particular setting and decide whether or not to add the device to an “approved” or “approved with mitigation” list developed by your program. Elastomeric Pumps in Hyperbaric Settings We are aware of several published reports of the performance of other elastomeric pumps in hyperbaric settings. Some results show a safe delivery of the medications with no adverse outcomes. Other reports with a separate make and model show a slight decrease in delivery rate. The UHMS HBO2 Safety Committee has responded to a similar question about the Braun Easypump several years ago. In your case, the information received by that manufacturer should provide some assurance that the pump will function as it was designed. Response and General Approach to Equipment Evaluation We would encourage you to first determine the necessity of the item for the time duration required to complete the therapy. Oftentimes, antibiotics may be delayed or briefly interrupted without negative outcomes. If it is possible and safe to delay either the HBO Therapy or the infusion, we would recommend this approach. If you are considering the option to test this device for safe use within the hyperbaric environment, we can provide you with specific resources that may assist you in your evaluation process. This information not an endorsement by the UHMS HBO2 Safety Committee for the use of this device in the hyperbaric environment. Rather, we hope that you will consider these suggestions in your individual approach: We strongly encourage a formal risk assessment of the device, with assistance from your hospital biomedical engineering group and perhaps your hospital safety or legal teams. If you discover that the device has been tested previously under hyperbaric conditions, we suggest that this may be utilized as validation of your final assessment, but we do not recommend that this is the entirety of device approval. Simply put, we recommend a formal risk assessment regardless of testing methods. (Exception: Modern ICD’s and Pacemakers are commonly tested by the manufacturer for function under pressure. Therefore, use under increased atmospheric conditions does not constitute an off-label use of those devices.) Consider reaching out to the manufacturer to learn more about the device, especially if there are limited performance details/specifications in the product manual. Try to gain an understanding of what types of stress the device was subjected to during the manufacturing and testing phase. You may wish to make the manufacturer aware of your intentions or you may remain anonymous. Regardless of the manufacturer’s response, there may be good reason for you to proceed with the evaluation, as this device may be vital to the continuum of care to the patient. It should be noted that any modifications to the device or use other than as recommended by the manufacturer risks voiding any warranty on the product. If evaluating a medical device, it is understood that few are intended to be used in the Multiplace hyperbaric environment. Therefore, consider that such use will likely fall into the FDA category of "Off-Label" and Investigational Use Of Marketed Drugs, Biologics, and Medical Devices “. You may also wish to review gov: Frequently Asked Questions about Medical Devices for more information. NOTE: Regarding medical device evaluation, at least one major academic institution’s legal team with experience in medical device modification has approached the current FDA regulations in the following fashion: “The program (modification and testing of medical devices for safe use in the hyperbaric environment) is not subject to FDA regulation. FDA regulates manufacturers and not the practice of medicine. Physicians are able to use FDA approved products other than under the labeled indications as long as the physician meets certain criteria. FDA’s statement on this off-label use is as follows: “Good medical practice and the best interests of the patient require that physicians use legally available drugs, biologics and devices according to their best knowledge and judgment. If physicians use a product for an indication not in the approved labeling, they have the responsibility to be well informed about the product, to base its use on firm scientific rationale and on sound medical evidence, and to maintain records of the product's use and effects. Use of a marketed product in this manner when the intent is the "practice of medicine" does not require the submission of an Investigational New Drug Application (IND), Investigational Device Exemption (IDE) or review by an Institutional Review Board (IRB).” We hope that this response will assist you in determining the best course of action for your program. Please do not hesitate to reach out to the UHMS HBO2 Safety Committee if you have any follow-up questions. Respectfully, The UHMS HBO2 Safety Committee REFERENCES: Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc. Burman F, Sheffield R, Posey K. Decision process to assess medical equipment for hyperbaric use. Undersea Hyperb Med. 2009;36:137–44. PMID: 19462753. Burnett, T., Bhalla, T., Sawardekar, A., & Tobias, J. D. (2011). Performance of the On‐Q pain infusion device during changes in environmental temperature. Pediatric Anesthesia, 21(12), 1231-1233. Cooper, N (Email Correspondence), “C-Series Info,” AVANOS Corporation. Received 3/24/23 Dohgomori, H., Arikawa, K., Gushiken, T., & Kanmura, Y. (2002). Accuracy of portable infusers under hyperbaric oxygenation conditions. Anaesthesia and intensive care, 30(1), 25-28. Lewis, I., Smart, D., Brown, B., & Baines, C. (2015). Performance of the Baxter Infusor LV10 under hyperbaric conditions. Diving Hyperb Med, 45, 37-41. Millar, I. L. (2015). Hyperbaric intensive care technology and equipment. Diving Hyperb Med, 45(1), 50-56. National Baromedical Society, “Flow Rate of the On-Q PainBuster under Hyperbaric Pressure,” Authored 7/19/2006. National Fire Protection Agency (NFPA). (2021). NFPA 99 2021 Edition: Health Care Facilities Code. Quincy, Massachusetts. https://www.nfpa.org/ Perks, S., Blake, D. F., Young, D. A., Hardman, J., Brown, L. H., Lewis, I., & Pain, T. (2017). An assessment of the performance of the Baxter elastomeric (LV10) Infusor™ pump under hyperbaric conditions. Diving and Hyperbaric Medicine, 47(1), 33. Radcliffe, J. J., & Spencer, I. (1994). Performance of the Baxter disposable patient‐controlled analgesia infusor under hyperbaric conditions. Anaesthesia, 49(9), 796-797. Salman, D., Barton, S., & Nabhani-Gebara, S. (2013). Effect of environmental conditions on performance of elastomeric pumps. American Journal of Health-System Pharmacy, 70(13), 1100-1100. Tobias, J. D., Johnson, G. A., & Patel, M. (2011). Performance of the On-Q pain infusion device during hyperbaric therapy. Anesthesia & Analgesia, 113(2), 275-277. US Food and Drug Administration. (2014). “Off-label” and investigational use of marketed drugs, biologics, and medical devices: information sheet. Silver Spring, MD. LINK Wang, J. (2013). Effect of environmental conditions on performance of elastomeric pumps--author's reply. American Journal of Health-system Pharmacy: AJHP, 70(13), 1100-1101. Workman, W. T., & Wood, J. S. (2020). Hyperbaric Facility Safety: A Practical Guide (2nd ed.). Best Publishing Company. DISCLAIMER Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.Any concerns with Fentanyl patch in monoplace chambers? Any risk of fire or effect on the delivery rate of fentanyl to the patient from pressure?
Posted: 4/7/2023
Q:
Any concerns with Fentanyl patch in monoplace chambers? Any risk of fire or effect on the delivery rate of fentanyl to the patient from pressure?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
We understand that there are many hyperbaric programs that allow Fentanyl and other medication patches, in the Class B Monoplace environment, and some that do not. The decision of the Medical Director and Safety Director of your program to allow should be based on a risk assessment of the product. The chief concerns are flammability and the potential for increased medication uptake.
With respect to the risk of fire, there is little data on the fire risk of transdermal patches. In an attempt to evaluate safety, Lavonas (2006) reviewed the results of a structured literature search, performed an analysis “of the potential for creating fire in the hyperbaric environment was performed using standard chemical and hazardous materials references and formulae at a range of appropriate pressure and FO2 values” and reviewed data from product manufacturers. The results of this study suggest the risk of fire from transdermal patches to be low in both multiplace and monoplace environments (Lavonas, 2006).
Regarding the potential risk of increased medication uptake, this concern is largely based in theory. There are no published evidence-based studies to suggest otherwise. Historically, the concern has been erratic or unpredictable drug absorption rates due to vasoconstriction and adiabatic temperature changes in the hyperbaric environment. One study that examined the effects of scopolamine patches on navy scuba divers found that “no unusual symptoms were seen as function of drug, pressure, or their interaction” (Schwartz, Curley, 1986).
Insight from the experience of our Safety Committee members:
- This question has come and gone for years. Many years ago we removed all patches. For the last 20+ years we have not. We have not observed problems.
- We have always removed them.
- It has been our practice to remove these patches.
- For patients hospitalized in our Intensive Care Unit (part of the Hyperbaric Center), we occasionally use patches with buprenorphine - without any adverse effects during HBOT.
- I cannot recall details, but once upon a time, I heard rumors that after a hyperbaric session in a multiplace chamber (in the other hyperbaric facility), there was red skin under the fentanyl patch, which was interpreted as skin burn due to increased temperature of the patch. Since then, we have been informing patients about this issue, asking them to observe local skin and the pharmacological effect of any patch (analgesic, nicotine, etc).
- I’ve heard the story of the multiplace chamber that got a nurse pregnant because her birth control patch didn’t work appropriately, and nobody told her about the issue while she worked in the chamber, but I’ve never seen this stated or reported in writing anywhere…just an anecdotal story.
- We’ve had no issues with transdermal patches that are gel-based at the dermal interface (e.g., Scopolamine)* or plastic membrane at the dermal interface (e.g., Fentanyl, Nicoderm CQ). The flammability risk was deemed low due to the sealing against the dermal surface and there have been no apparent dosing changes concurrent with HBO pressure changes.
- There is an August, 2014 article reporting two cases of no harm using daily removal (for HBO) and daily re-application of transdermal Fentanyl patches. (Pawasauskas & Perdrizet, 2014)
- I seem to remember receiving training somewhere that transdermal patches with foil dermal interfaces can have their pores altered such that an increased dose is delivered in hyperbaric conditions, but I can’t find that training or any examples of foil transdermal patches. I believe some of the estrogen birth control patches are of this type. There was a 2005 diving discussion board post about this and other transdermal patches with a response from DAN that indicated no dose change would be expected from pressure, but one could be expected from increased temperature water activities such as hot tubs. https://scubaboard.com/community/threads/ortho-evra-birth-control-patch-and-diving.83555/
- We talk about vasoconstriction and vasodilation due to the pressure, but few take into account the ambient temperatures which regulate drug absorption as well. I’m going to posit that these cancel each other . And, we do not prohibit patients with patches going out in 110F temp, or the other extreme 0F. There are no publish studies showing over/under dosing due to ambient temperatures.
- As long as the patient is not compromised on the daily pre-HBOT evaluation, I see no problem leaving the Fentanyl patch in place. I have heard all kinds of arguments for/against, but there isn’t one shred of evidence in the literature. Two articles: Lavonas found that these are not fire risks, and one other paper that removed patches every day and replaced with a fresh patch safely, which raises several other questions:
- Who in your clinic can remove/replace drug elution patches?
- What do you do with the patch you just removed? Do you replace the same patch after each treatment (these are 72-hr patches)
- Who answers to the physician state board of dependent drugs for going through a patch every day?
- So, the answer will be whatever your habit is … without much science. Mine is … I left the patches in place. Never had a patient over-dose during any HBOT treatment.
- I don’t see any fire and clearly no mechanical issues. I checked a SDS and it indicates the product being non-flammable.
- We’ve allowed this patch for 10+ years with no reported adverse effects.
As indicated by the comments above, there is no consensus agreement. Fortunately, there are many studies and case reports available to assist program leaders in making the best decision for their particular practice. We encourage you to review these resources below.
Respectfully,
The UHMS HBO2 Safety Committee
REFERENCES:
- Lavonas, E.J. (2006). Safety analysis of transdermal medication delivery systems in the hyperbaric environment [Abstract]. Undersea and Hyperbaric Medical Society.
- Schwartz, H.J.C., Curley, M.D. (1986). Transdermal scopolamine in the hyperbaric environment [Abstract].
- Mikaili P, Moloudizargari M, Aghajanshakeri S. (2014). Treatment with topical nitroglycerine may promote the healing process of the diabetic foot ulcers. Medical Hypotheses, 83(2), 172-174. doi: 10.1016/j.mehy.2014.05.002.
- Coto-Segura, P., Ingelmo, J., Alonso, T., Sanchez-Sambucety, P., Rodriguez-Prieto, M.A. (2007). Effectiveness of topical application of nitoglycerin spray to increase survival of cutaneous flaps and grafts. Actas Demosifilogr, 98, 291-5.
- Coruh, A., Abaci, K., Gunay, G.K. (2004). Effect of topical nitroglycerine on the survival of ischemic flow-through venous flaps in rabbits. Journal of Reconstructive Microsurgery, 20(3):261-6.
- Hotkar, M.S., Avachat, A.M., Bhosale, S.S., Oswal, Y.M. (2013). Preliminary investigation of topical nitroglycerin formulations containing natural wound healing agent in diabetes-induced foot ulcer. Internation Wound Journal, ISSN 1742-4801.
- Pawasauskas, J., Perdrizet, G. (2014). Daily application of transdermal fentanyl patches in patients receiving hyperbaric oxygen therapy. Journal of Pain & Palliative Care Pharmacotherapy, 28, 226-232.
- Williams, T. H., Wilkinson, A. R., Davis, F. M., & Frampton, C. M. (1988). Effects of transcutaneous scopolamine and depth on diver performance. Undersea biomedical research, 15(2), 89–98.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is the Biotronik Iperia 7 DR-T safe for HBO exposure? The manufacturer says: Hyperbaric oxygen therapy (HBOT) for patients with BIOTRONIK CRM devices is not recommended due to the potential for damage or impaired function of the implant after exposure. The physician should conduct a risk-benefit analysis if HBOT treatment is necessary. BIOTRONIK CRM devices are tested at various ambient pressures. The testing conditions vary between different device types and generations; however, device damage has never
Posted: 5/1/23
Q:
Is the Biotronik Iperia 7 DR-T safe for HBO exposure? The manufacturer says: Hyperbaric oxygen therapy (HBOT) for patients with BIOTRONIK CRM devices is not recommended due to the potential for damage or impaired function of the implant after exposure. The physician should conduct a risk-benefit analysis if HBOT treatment is necessary. BIOTRONIK CRM devices are tested at various ambient pressures. The testing conditions vary between different device types and generations; however, device damage has never been experienced as a result of exposure to HBOT. The following product families have been tested in compliance with ISO 14708-2:2012: Edora, Enitra, Enticos, Evity pacemakers and CRT-Ps 40 cycles1 of ambient pressure up to 304 kPa (3.04 bar).
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
The UHMS HBO2 Safety Committee is not able to endorse hyperbaric exposure of an implanted pacemaker or defibrillator that has not been pressure-tested by the manufacturer to at least the maximum intended treatment pressure.
However, this is a medical decision to be made by the Hyperbaric Medical Director with technical input and risk assessment from the Hyperbaric Safety Director. The manufacturer has indicated that while not tested, they are aware that their devices have been used, and that no adverse events have been reported. If your physician determines that the potential risks are warranted, we recommend that the decision is documented clearly in the patient’s chart and the patient is made aware of the potential risk of damage to the device caused by increased atmospheric pressure that could lead to failure of the device.
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc. LINK
- National Fire Protection Agency (NFPA). (2021). “NFPA 99 2021 Edition: Health Care Facilities Code.” Quincy, Massachusetts. LINK
- Workman, W. T., & Wood, J. S. (2020). Hyperbaric Facility Safety: A Practical Guide (2nd ed.). Best Publishing Company. LINK
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is there a portable pulse ox that would be safe for a monoplace chamber? Thinking similar to an onyx style device.
Posted; 11/1/23
Q:
Is there a portable pulse ox that would be safe for a monoplace chamber? Thinking similar to an onyx style device.
A :
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/HSC) of your facility.
When approaching the prospect of any item in a hyperbaric environment, especially the 100% oxygen environment of a typical monoplace chamber, it is important to weigh the risk of the device versus the benefit gained from allowing the device to be used. In this instance the consensus agreement of the UHMS HBO2 Safety Committee is that pulse oximetry values are not a necessary vital sign within the clinical setting during administration of hyperbaric oxygen therapy. Given the fact that the patient is breathing 100% oxygen, it would be reasonable to assume that the patient’s hemoglobin will remain fully saturated while therapy is underway. Additionally, the delivery of hyperbaric oxygen therapy affects the capacity of blood plasma to take on increasing levels of oxygen molecules, thereby nearly surpassing the need for hemoglobin altogether.
From a research standpoint, we are unaware of pulse oximeter testing in an oxygen-enriched or near 100% oxygen environment, although studies have been conducted in a pressurized air environment. We will cite a few articles of possible interest for your review.
- The Navy Experimental Diving Unit (NEDU) tested the Nonin models 8500, 9500, and 9847 pulse oximeter in 2004; testing was conducted in an air environment – not oxygen.
- Suitability of Ohmeda Model 3775 Pulse Oximeter for use in Hyperbaric Chambers was published in 1999 by NEDU; testing was likely conducted in an air environment – not oxygen.
Testing these devices in an environment of enriched oxygen would be challenging. Citations from NFPA 99 2024 containing additional requirements for a Class B chamber are outlined below.
14.2.9.6 Additional Wiring and Equipment Requirements Inside Class B and Class C Chambers.
The requirements in 14.2.9.6 shall apply to Class C chambers pressurized with oxygen and to Class B chambers whether they are pressurized with oxygen or with air.
14.2.9.6.4
Equipment not specified by 14.2.9.6 shall be permitted in the chamber, with the approval of the hyperbaric medical director and the hyperbaric safety coordinator, if any of the following conditions exists:
- The equipment is intrinsically safe.
- The equipment is compliant with Class 1 requirements specified in Article 500 of NFPA 70.
- The equipment meets all of the following conditions:
- The batteries and circuitry are sealed or isolated from the chamber environment.
- The equipment has a maximum voltage of 3 volts and a power requirement of 4 W.
- The equipment contains no volatile lubricants or hydrocarbons.
Once again, we encourage you to weigh the risk versus benefit, while considering that this is not a common practice among monoplace hyperbaric providers nationally, due to the inherent dangers that are present. Please reach out to us if you have any follow-up questions.
Respectfully,
The UHMS HBO2 Safety Committee
REFERENCES:
- Burman, F. (2019). Risk assessment guide for installation and operation of clinical hyperbaric facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- Latson, G. W. (2004). Suitability of Nonin models 8500 and 9500 pulse oximeters, and model 9847 pulse oximeter, and carbon dioxide detector for use in hyperbaric chambers (NEDU TR 04-06). Navy Experimental Diving Unit.
- NFPA 99. (2023). NFPA 99 Heath care facilities code (2024 ed.) National Fire Protection Association.
- Perez-Vidal, C., Gracia, L., Carmona, C., Alorda, B., & Salinas, A. (2017). Wireless transmission of biosignals for hyperbaric chamber applications. PloS one, 12(3), e0172768.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Are polypropylene eye lash extensions contraindicated?
Posted: 11/8/2023
Q:
Are polypropylene eye lash extensions contraindicated?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/HSC) of your facility.
The UHMS HBO2 Safety Committee does not consider eye lash extensions to be contraindicated to hyperbaric therapy. However, we encourage each facility’s HMD and HSD/HSC to evaluate and document items for safety within the hyperbaric environment.
You may wish to review a previously answered MEDFAQ related to hair extensions, where the documentation and risk assessment of such products is described.
REFERENCES:
- Burman, F. (2019). Risk assessment guide for installation and operation of clinical hyperbaric facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- NFPA 99. (2023). NFPA 99 Heath care facilities code (2024 ed.) National Fire Protection Association.
- UHMS HBO2 Safety Committee, MEDFAQ Response, “Hair Weave or extensions with Keratin glue” Published 10/2015.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
As the use of hair extensions continues to rise, Kanekalon has emerged as the predominant material choice. I came across a website that has conducted flame testing on this material, and I'm interested in hearing the safety committee's perspective on it. https://www.kanekalon-hair.com/en/lineup
Posted: 11/22/23
Q:
As the use of hair extensions continues to rise, Kanekalon® has emerged as the predominant material choice. I came across a website that has conducted flame testing on this material, and I'm interested in hearing the safety committee's perspective on it. https://www.kanekalon-hair.com/en/lineup
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/HSC) of your facility.
Although it is notable that the test data claims the material to be self-extinguishing, flame-retardant, and having a limited oxygen index, these tests were performed at sea level within an air (21% oxygen) environment. It is the Safety Committee’s view that those tests should not be viewed as relevant when evaluating this product for exposure to 100% oxygen under pressure. It is improper to apply this data to the much different environment of the Class B monoplace chamber, or within an oxygen hood used in a Class A multiplace chamber. Remember that in an oxygen-enriched environment under pressure, the autogenous ignition temperature (AIT) will likely be lower, the flame-spread rate will be exponentially faster, and flame-retardant attributes will decrease significantly thereby eliminating the self-extinguishing properties.
A key factor for the HSD/HSC when making these decisions is knowing the materials that may be on or in the product so you may mitigate the risks appropriately. Consider the adhesive used with the extensions; Is it completely dry and free of vapor? What about other hair products (hairspray, gel, oils, etc.)? In our view, this is a greater concern than Kanekalon® itself, due to the potential for flammable vapors to be present. The NFPA states:
14.3.1.6.5 The use of flammable hair sprays, hair oils and skin oils shall be prohibited for all chamber occupants/patients as well as personnel.
14.3.1.6.5.2 All cosmetics, lotions, and oils shall be removed from the patient’s body and hair.
We understand the importance of conformity to the code standard listed above. To address the possibility of residual vapors that may be present, we suggest that the hair extensions be wrapped with a 100% terrycloth cotton towel dampened with clean fresh water (not saline). The use of 100% terrycloth cotton allows for maximum containment of water due to its unique loop design.
If treatment in a Class A multiplace chamber is necessary, you may wish to utilize a face mask vs the oxygen hood to achieve a greater safety margin.
Whether they have hair extensions or not, all hyperbaric patients must be made aware of the risk of exposing flammable agents into the chamber. Before each treatment, proper screening by hyperbaric staff is necessary to ensure that patients meet the conditions for treatment. Patients must be informed of the approach the team will take if prohibited items/flammable agents are found during the pre-treatment process.
Finally, it is important for staff members to trust their nose and eyes during screening, and to stay vigilant. Keep in mind that patients rely on you, the Hyperbaric Professional to screen them properly. While it is considered positive to have a trusting relationship with your patient, we warn you to guard against complacency. Avoid thoughts like “They’ve done this a thousand times, I’m sure that they are safe,” and “We are running late, do I really want to bother the patient again and have them remove the rest of their makeup? ”
A good rule of thumb is to approach each treatment as if it is the patient’s very first treatment. You may find it helpful to recall how you behaved the first time you conducted a safety time-out.
Respectfully,
The UHMS HBO2 Safety Committee
REFERENCES:
- Burman, F. (2019). Risk assessment guide for installation and operation of clinical hyperbaric facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- NFPA 99. (2023). NFPA 99 Heath care facilities code (2024 ed.) National Fire Protection Association.
- UHMS HBO2 Safety Committee, MEDFAQ Response, “Hair Weave or extensions with Keratin glue” Published 10/2015.
- UHMS HBO2 Safety Committee, MEDFAQ Response, “Polypropylene Eye Lashes” Published 10/2023.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is use of water treatment additive for HBO monoplace unit portable humidifier allowed? Additive is made of 2-phosphonobutane-1,2,4-tricarboxylic acid (1-5%), quaternary ammonium compounds, benzyl-C12-16-alkyldimethyl, chlorides (1-5%) & sodium hydroxide (0.1-1%).
Posted: 1/2/24
Q:
Is use of water treatment additive for HBO monoplace unit portable humidifier allowed? Additive is made of 2-phosphonobutane-1,2,4-tricarboxylic acid (1-5%), quaternary ammonium compounds, benzyl-C12-16-alkyldimethyl, chlorides (1-5%) & sodium hydroxide (0.1-1%).
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
We understand that your facility is utilizing a humidifier within the room housing two Monoplace chambers, which some facilities use to reduce static accumulation. Based on the chemicals mentioned, we are assuming that this additive is necessary to prevent algae or bacteria from forming and presenting a health risk to the occupants in the room.
The Safety Committee does not see that there is an increased risk of fire caused by vaporization of the additive, instead, most members of the Committee considered the possibility of damage to acrylic surfaces. We presented your question to a representative from a well-known manufacturer of acrylic and this was their response (G. Richard, personal communication, December 11, 2023):
“Although I do not have the SDS for the product, I have reviewed the ingredients and can confirm that they are all highly water soluble and at the concentrations specified are most unlikely to harm acrylic windows.
Our acrylic is regularly exposed to 15% aqueous sodium hydroxide when cleaning chromatography media used to produce Insulin and mRNA protein-based drugs. At between 1% to 5% it is too water soluble to damage acrylic and is used to prevent Calcium salt crystallization from hard water.
Quaternary ammonium compounds, benzyl-C12-16-alkyldimethyl are simple surfactant molecules - again totally compatible with acrylic.
0.1% to 1% sodium hydroxide solution would again not be a problem - even when combined with the other ingredients.
I do recommend that you determine whether there is a volatile organic compound (VOC) present in the formulation - e.g. ethanol, isopropanol, benzyl alcohol or Dowanol - ethylene glycol monobutyl ether. Unlikely but these solvents - even at low concentrations can damage acrylic.”
Based upon this viewpoint and discussion among Committee members, we would suggest that you explore the SDS of this product further to identify any Volatile Organic Compounds. If these are present, we would caution against using the use of this specific additive within the room housing the chambers. The UHMS HBO2 Safety Committee has answered several related questions to humidity and static (listed below). We hope this will help guide your risk assessment and decision making surrounding this topic.
Respectfully,
UHMS HBO2 Safety Committee
BIBLIOGRAPHY:
- Undersea and Hyperbaric Medical Society, MEDFAQ Response, “Humidity in the room housing monoplace chambers,” Accessed 12/15/2023.
- Undersea and Hyperbaric Medical Society, MEDFAQ Response, “Observation of static buildup within a monoplace chamber,” Accessed 12/15/2023.
- Wood, J. S. (2020). Static electricity. In W.T. Workman, & J. S. Wood (Eds.) Hyperbaric facility safety: A practical guide (2nd ed., p. 313). Best Publishing Company.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
We have a patient who is currently getting HBO for a DFU and had Mirragen® Bioactive Glass applied to his wound. This a new skin substitute to our clinic and I am not familiar with it. Do you know if this is HBO approved?
Posted: 1/22/2024
Q: We have a patient who is currently getting HBO for a DFU and had Mirragen® Bioactive Glass applied to his wound. This a new skin substitute to our clinic and I am not familiar with it. Do you know if this is HBO approved?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
Members of the Safety Committee have reached out to the manufacturer, but have not received any feedback. We have reviewed all of the relevant documentation that we could find on this product, to include the FDA’s Premarket notification documents, instructions for use, and independent references providing public information wound care products.
Our review has not uncovered a significant reason to cause concern for increased fire risk in the monoplace or multiplace hyperbaric environment. It is our understanding that Mirragen© is composed of natural body elements including Calcium, Boron, Magnesium and Phosphorus. These elements are contained within the dressing and are absorbed by the body.
This assessment is the opinion of the Hyperbaric Safety Committee and does not constitute product approval. We suggest that the HMD and HSD/C of your facility perform a risk assessment and document your conclusions prior to treating the patient.
Respectfully,
UHMS HBO2 Safety Committee
BIBLIOGRAPHY:
- Burman, F. (2019). Risk assessment guide for installation and operation of clinical hyperbaric facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- NFPA 99. (2023). NFPA 99 Heath care facilities code (2024 ed.) National Fire Protection Association.
- FDA 510(k) resource page, US Food and Drug Administration. Accessed January 17, 2024. LINK
- Engineered Tissue, Inc., “Mirragen – Instructions for Use.” Accessed January 17, 2024. LINK
- Woundsource Product Guide, “Mirragen Bioactive Glass.” Accessed January 17, 2024. LINK
DISCLAIMER Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Has anyone come across BioPatch made by Ethicon? It is a sponge impregnated with chlorhexidine gluconate. I don't note any glaring indication why it can't be keep in place under tegaderm in a monoplace chamber but wanted to know if anyone else has come across this product. Thank you.
Posted: 1/22/24
Q: Has anyone come across BioPatch made by Ethicon? It is a sponge impregnated with chlorhexidine gluconate. I don't note any glaring indication why it can't be keep in place under tegaderm in a monoplace chamber but wanted to know if anyone else has come across this product.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
Members of the Safety Committee have reviewed the relevant documentation that we could find on this product, to include the FDA’s Premarket notification documents, instructions for use, Safety Data Sheet, and independent references providing public information wound care products.
Our review has not uncovered a significant reason to cause concern for increased fire risk in the monoplace or multiplace hyperbaric environment. It is our understanding that BioPatch© is a protective sponge impregnated with chlorhexidine gluconate and is usually covered with Tegaderm©.
This assessment is the opinion of the Hyperbaric Safety Committee and does not constitute product approval. We suggest that the HMD and HSD/C of your facility perform a risk assessment and document your conclusions prior to treating the patient.
Respectfully,
UHMS HBO2 Safety Committee
BIBLIOGRAPHY:
- Burman, F. (2019). Risk assessment guide for installation and operation of clinical hyperbaric facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- Ethicon, Inc., “BIOPATCH with CHG – Instructions for Use.” Accessed January 17, 2024. LINK
- FDA 510(k) resource page, US Food and Drug Administration. Accessed January 17, 2024. LINK
- HR® Pharmaceuticals, Inc., “Safety Data Sheet – Chlorhexidine Gluconate.” LINK
- Johnson & Johnson Med Tech, “BIOPATCH Brochure.” Accessed January 17, 2024. LINK
- NFPA 99. (2023). NFPA 99 Heath care facilities code (2024 ed.) National Fire Protection Association.
DISCLAIMER Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is it safe to use a Medtronic MiniMed 780G CGM with Guardian 4 sensor in a monoplace chamber?
Posted: 2/12/2024
Q: Is it safe to use a Medtronic MiniMed 780G CGM with Guardian 4 sensor in a monoplace chamber?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
The UHMS HBO2 Safety Committee is not aware of any pressure tolerance testing or safety evaluation of this particular model. A member of the Committee has reached out to the Medtronic Technical team. They did not indicate that this device has undergone testing, nor did they reveal any plans to do so.
The UHMS HBO2 Safety Committee does not recommend use of the MiniMed 780G monitor or the Guardian 4 Sensor in the Monoplace hyperbaric environment.
Respectfully, UHMS HBO2 Safety Committee
DISCLAIMER Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members can provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and hyperbaric safety director/coordinator of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Does anyone have any experience with a person who ingests a PILLcam for VCE prior to HBOT? We are treating someone for radiation enteritis who just took one and it sounds as if it included a battery with a life of 12 hours. I am uncertain how long it takes for it to pass after. Since it is ingested, would it matter?
Posted: 3/11/2024
Q: Does anyone have any experience with a person who ingests a PILLcamtm for VCE prior to HBOT? We are treating someone for radiation enteritis who just took one and it sounds as if it included a battery with a life of 12 hours. I am uncertain how long it takes for it to pass after. Since it is ingested, would it matter?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
The Safety Committee does not see any immediate safety concerns regarding the presence of this device in the human body while undergoing hyperbaric therapy. From what we know about this product, the casing is soft and should not collapse. Also, it is important to keep in mind that the item was designed to be ingested and pass through the gastrointestinal tract, so it is reasonable to consider that it will likely survive exposure to changes in pressure. According to the American Society for Gastrointestinal Endoscopy, the device should pass through the body within 2 weeks. If it does not, then further investigation is in order.1
The manufacturer has reported that the acceptable operating pressure range is 10.2 - 15.4 psia (0.69 – 1.05 ATA). We suspect that this was tested to ensure a hermetic seal (autoclaving). The shell does contain a number of parts to include batteries (see photos).
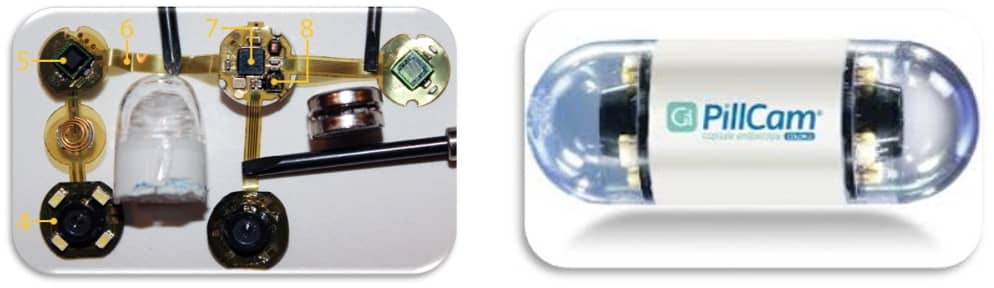
Following a documented risk assessment, some facilities choose to wait until the PillCamtm passes prior to undergoing elective hyperbaric oxygen therapy. In the event of emergent hyperbaric therapy, some practices offer therapy with informed consent.
Respectfully,
UHMS HBO2 Safety Committee
REFERENCE/S: (Use for information necessary to identify and retrieve each work cited in the text above.)
- American Society for Gastrointestinal Endoscopy. Video Capsule endoscopy. GASTROINTESTINAL ENDOSCOPY Volume 93, No. 4 : 2021 LINK
- Medtronic Corporation. Storage and Operating Pressure. Pillcam SB 3 Capsule Endoscopy System. Accessed 3/11/2024 LINK
BIBLIOGRAPHY: (Use for background or further reading.)
- Burman F. Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities. 6th ed. San Antonio: International ATMO, Inc; 2019.
National Fire Protection Association. NFPA 99 2024 Edition: Health Care Facilities Code. Quincy; 2024.
DISCLAIMER Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members can provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and hyperbaric safety director/coordinator of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is it safe to allow a CENTRAK Real Time Tracking Device in the Multiplace Hyperbaric Chamber?
Posted: 3/20/2024
Q: Is it safe to allow a CENTRAK Real Time Tracking Device in the Multiplace Hyperbaric Chamber?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
The UHMS HBO2Safety Committee is aware of facilities that have allowed similar real-time tracking devices in the multiplace chamber. We are not aware of any facilities that have allowed this particular device. In any case, we suggest conducting a thorough risk assessment(1), utilizing resources you have in your institution (i.e. safety officers, biomedical technicians, electrical engineers, etc.). The UHMS HBO2 Safety Committee can provide guidance to assist your decision making but cannot endorse a specific product for use. The following approach may be beneficial in your assessment as applicable; it applies to most electrical devices considered for use.
Question #1: Is it necessary?
Allowing any electrical device into a pressurized environment carries risk. First, your leadership team (at minimum, the HMD and HSD/C) must determine if the device is necessary for patient care. If your facility requires these tracking devices, you’ll want to list the risk areas as described in the NFPA 99, chapter 14(4) in relation to portable, battery-powered equipment.
The UHMS HBO2 Safety Committee suggests reviewing several risk areas, posed as questions below. Please keep in mind that this is not an all-inclusive list.
Question #2: Will it generate heat?
The NFPA 99, Chapter 14(4) identifies that electrical equipment installed or used in the chamber have an operating surface temperature less than 85°C (185°F) (14.2.9.3.11)
Question #3: Does the battery meet requirements?
NFPA 99, Chapter 14(4) identifies that:
- Batteries must be fully enclosed and secured within the device. (14.2.9.3.16.4(1)).
- Batteries must not be damaged by the maximum chamber pressure they are exposed to (14.2.9.3.16.4(2))
- Batteries must be of a sealed type that does not off-gas during normal use. (14.2.9.3.16.4.(3))
- The batteries or battery-operated equipment are not charged while located in the chamber. (14.2.9.3.16.4(4)). Clearly this does not apply to disposable batteries that are used in the device you are enquiring about (3).
- The batteries are not changed on in-chamber equipment while the chamber is in use. (14.2.9.3.16.4(5))
- The electrical rating of the device is less than 12V and 48W. (14.2.9.3.16.4(6))
You may consider replacing the battery more frequently than the manufacturer’s requirement and increasing the frequency of any required Preventative Maintenance (likely none as these are typically replaced periodically).
Important Distinction: Disposable Lithium vs. Rechargeable Lithium-Ion
Of note, the batteries that appear to be used in the CENTRAK Model ITD-761E H (Rev E) are low-voltage disposable lithium thionyl chloride batteries (3.6V) and should be relatively risk-free. The risk profile of these batteries is much lower than that of a rechargeable lithium-ion battery. However, awareness of the potential for internal or external short-circuits, which can result in high heat releases, together with toxic emissions, should remain in place.
Rechargeable lithium-ion batteries have not been prohibited within the hyperbaric chapter of the NFPA 99 Code since the 2015 version, provided that they meet the requirements of section 14.2.9.3.16.4. It is important to understand that lithium-ion batteries may carry a higher risk if a short-circuit occurs, either external or internal, and resulting in a significant release of heat(2).
Question #4: Does the device pose a risk of shock?
It is important to ascertain that the internal components are reasonably protected from water, and that any electrically conductive casings of all portable equipment for use inside the chamber are grounded. (1 4.2.9.3.8)
Question #5: Will it function under pressure and following rapid pressurization/rapid decompression?
Modern devices often utilize air-filled buttons to power on and off the device, and keypad entry. Beware of any potential for trapped air within the compartment which could cause a malfunction. Following pressure testing, you may wish to send the device to the manufacturer for their input/assessment, if they are willing.
In addition to these risk areas, we would suggest that hyperbaric staff receive training related to the use of the device and ensure that equipment is visually inspected for damage prior to use. We would suggest that any device that is routinely utilized be part of an ongoing maintenance program.
Respectfully,
UHMS HBO2 Safety Committee
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- Burman, F. (2020). Use of Lithium‐Ion Batteries in Hyperbaric Chambers. San Antonio, TX: International ATMO, Inc.
- Coincell Battery Solutions, “Product Specification: LI-socl2 battery, model ER14250H,” Published March 2017
- National Fire Protection Association. (2024). NFPA 99 2024 Edition: Health Care Facilities Code. Quincy, Massachusetts.
BIBLIOGRAPHY:
- Chimiak, J. (2010). Evaluating Equipment and Materials for Use in a Hyperbaric Oxygen Environment: Clinical Hyperbaric Evaluation and Testing (CHET) Program. (3rd ed.). Best Publishing Company.
- Undersea and Hyperbaric Medical Society – Hyperbaric Oxygen Safety Committee (2023), “Medical Device Approval Form – Multiplace” LINK
- Workman, W. T., & Wood, J. S. (2020). Hyperbaric Facility Safety: A Practical Guide (2nd ed.). Best Publishing Company.
- CenTrak, Inc., “Technical Specifications: IT-761,” Published 2012, Accessed 2/14/2024.
DISCLAIMER Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members can provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and hyperbaric safety director/coordinator of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Can you provide feedback regarding the use of an AED immediately after removing a patient from the chamber during a cardiac event? Example Patient becomes unresponsive during treatment chamber is decompressed, and patient is removed from the chamber. Patient gown and linens are removed from the top of the patient and CPR is started, utilizing an AED. Question Can the patient remain on the chamber stretcher while utilizing the AED or does the patient need to be transferred to another not oxygenated surface
Posted: 3/20/2024
Q: Can you provide feedback regarding the use of an AED immediately after removing a patient from the chamber during a cardiac event? Example Patient becomes unresponsive during treatment chamber is decompressed, and patient is removed from the chamber. Patient gown and linens are removed from the top of the patient and CPR is started, utilizing an AED. Question Can the patient remain on the chamber stretcher while utilizing the AED or does the patient need to be transferred to another not oxygenated surface to use the AED if shockable rhythm is detected?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
In 2022, research was conducted regarding oxygen leaving a monoplace chamber to understand at which time and distance oxygen is sufficiently dispersed to conduct advanced cardiac life support on top of a mattress immediately removed from an oxygen-filled monoplace hyperbaric chamber.1 Information from this research was presented at the UHMS ASM Safety Pre-Course.2 Future studies plan to repeat this study with a manikin or patient present during testing.
The researcher recommends moving the gurney one gurney length away from the monoplace chamber; this may be accomplished by rotating the gurney 90o or backing the gurney away from the chamber. Relocating the gurney should provide sufficient access to the patient from responding teams. While relocating the gurney, it is essential to agitate the area to disperse any remaining oxygen. The quickest way to disrupt the remaining oxygen is to:
- Relocate the gurney one gurney length away from the chamber,
- Remove the patient’s blanket (or top sheet) and pillow, and
- Expose the chest.
During a medical emergency, leaving the chamber’s gurney attached to the chamber could limit access to one side of the gurney due to interference from the chamber’s door; therefore, it is reasonable to assume the gurney would be disconnected and moved away from the chamber door opening to allow unimpeded access to the patient. The combined movement of linen removal, gurney relocation, and staff activity should produce enough movement to disperse any oxygen remaining above 21%. Also, before attempting defibrillation, the correct placement of pads or paddles is necessary to avoid potential electrical arcing.
When designing an emergency procedure at an individual location, the Hyperbaric Safety Director/Coordinator, in consultation with the Hyperbaric Medical Director, should consider the impact ACLS could have on other patients undergoing hyperbaric therapy since the standard monoplace hyperbaric chamber is predominantly made of clear acrylic. The decision to move the affected patient to a separate room may be to keep other patients from witnessing a medical emergency.
Respectfully,
UHMS HBO2 Safety Committee
REFERENCE/S: (Use for information necessary to identify and retrieve each work cited in the text above.)
- Barry R. An Evaluation of Oxygen Dispersion When Released from a Monoplace Hyperbaric Chamber. Dissertation. Indiana University of Pennsylvania; 2022.
- Barry R. Where to defibrillate – In the HBO2 room or not? Presentation presented at: UHMS Annual Scientific Meeting Safety Pre-Course; June 15, 2023; San Diego, CA
BIBLIOGRAPHY: (Use for background or further reading.)
- Kindwall, E. P., & Goldmann, R. W. (1995). Hyperbaric medicine procedures. Department of Hyperbaric Medicine, St. Luke's Medical Center.
- Kindwall, E. P., & Niezgoda, J. A. (2006). Hyperbaric medicine procedures. Department of Hyperbaric Medicine, St. Luke's Medical Center.
- Weaver, L. K. (1995). Management of critically ill patients in the monoplace hyperbaric chamber, Hyperbaric Medicine Practice. Edited by Kindwall EP. Flagstaff.
- Weaver, L. (2008). Critical care of patients needing hyperbaric oxygen therapy. In: “Physiology and Medicine of Hyperbaric Oxygen Therapy”, Neuman, T.S., Thom, S.R., pg. 124.
DISCLAIMER Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members can provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and hyperbaric safety director/coordinator of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is it safe to allow Mastisol and Detachol in the Class B Monoplace Chamber?
Posted: 4/16/24
Q: Is it safe to allow Mastisol and Detachol in the Class B Monoplace Chamber?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
The Safety Committee recommends that a risk assessment be performed and documented by the Hyperbaric Safety Director/Coordinator of your facility. The Hyperbaric Medical Director should review this document and the two should jointly decide the course of action.
The Safety Committee has reviewed the SDS information pertaining to these products, and due to the presence of flammable vapors, do not recommend that these products be exposed under hyperbaric conditions in the Monoplace Class B environment in a liquid state. However, if these products have dried to the point where no vapor is present, it may be safe to allow. One way to assess this is to observe the presence of any odor from the application site.
Ignition of dried substances such as these require enough heat until vapors form, followed by sufficient heat to ignite the vapor. The UHMS Ad Hoc Materials Testing Advisory Committee (MTAC) was formed in 2017 to address questions related to materials in oxygen enriched environments. MTAC testing of adhesives found that while vapors ignited, it was not without significant manipulation of the variables (pressure, heat, time) beyond normal (and extreme) hyperbaric conditions.
Mastisol may be found in various adhesives used to make tape and bandages, which may be medically necessary to secure wound dressings and keep wounds clean. Detachol is an adhesive remover, and we recommend that areas of the skin where it was used is clean and dry prior to allowing the patient into the Monoplace Class B environment. As always, ensure that no ignition sources are present.
The Safety Committee recommends the same approach for these products in the Multiplace Class A environment. We will list several reference documents for your review.
Respectfully,
UHMS HBO2 Safety Committee
REFERENCE/S:
- Eloquest Healthcare, inc., “Safety Data Sheet – Detachol Adhesive Remover,” Accessed 4/15/2024 https://ferndalepharmagroup.com/wp-content/uploads/2015/02/Eloquest-Detachol-SDS.pdf
- Eloquest Healthcare, inc., “Safety Data Sheet – Mastisol Liquid Adhesive,” Accessed 4/15/2024 https://www.medline.com/media/catalog/Docs/MSDS/MSD_SDSD10436.pdf
BIBLIOGRAPHY:
- Burman, F. (2019). Risk assessment guide for installation and operation of clinical hyperbaric facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- NFPA 99. (2023). NFPA 99 Heath care facilities code (2024 ed.) National Fire Protection Association.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members can provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and hyperbaric safety director/coordinator of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
I am safety coordinator of a monoplace hyperbaric facility. I have a question regarding glucose administration during treatment. We are currently using glucose tablets mid treatment for some of our patients. One of these patients has poor fitting dentures that are removed pre-treatment. This prevents them from being able to chew the glucose tablet and results in them sucking on it for a prolonged time. The question has arisen is this too large of an aspiration risk. We have discussed switching to a
Posted: 7/10/24
Q: I am the safety coordinator of a monoplace hyperbaric facility. I have a question regarding glucose administration during treatment. We are currently using glucose tablets mid treatment for some of our patients. One of these patients has poor fitting dentures that are removed pre-treatment. This prevents them from being able to chew the glucose tablet and results in them sucking on it for a prolonged time. The question has arisen is this too large of an aspiration risk. We have discussed switching to a glucose gel as needed, but then the questions arose about what the packaging is made of and if that is safe in the chamber. I was wondering if there was any consensus on glucose gels in the monoplace environment?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
We are not aware of any consensus that has been reached by the hyperbaric community regarding a particular type of fast-acting glucose. We understand its purpose for emergency measures, but keep in mind that gels and other fast-acting simple sugars should not be used as a primary means to regulate blood glucose. This type of approach to glucose management may send a mixed message, as a quick spike in glucose can drop just as quickly as it rises(4), and these wide variations may not promote healing in a diabetic ulcer.
There may be several solutions to your concern. Many hyperbaric programs find it best to approach the issue of glycemic control by initiating an individualized treatment plan for each of their diabetic patients.(3) Routine evaluation of blood glucose levels is often part of this approach. In some cases where blood glucose levels are well—managed, it may not be necessary to include glucose in the chamber while treating a diabetic patient.(2,5)
Based upon your description of the patient, it appears that your aspiration concern is well-placed. Of course, we encourage you to consult with the Hyperbaric Physician prior to making any make any medical decisions regarding the delivery of glucose to the patient. Another method of glucose management to be considered is the administration of small sips of juice during therapy. There is the likelihood that that patient may not be able to comprehend the instructions necessary to administer a bolus of glucose gel by the time they show signs of needing it. This method allows for easier, more frequent, ingestion and reduces the aspiration risk associated with glucose tablets, especially for patients without dentures.
If it is deemed necessary to utilize glucose gel in the monoplace chamber, we do not see any significant physical safety concerns outside of the expansion of gases within a sealed container during decompression if the tube is opened at pressure and re-capped. When used, we advise directing the patient to rub a small amount of glucose gel on their gums or cheek as is typical in the prehospital setting. This method is described in several journal publications. One excerpt is quoted here for your convenience.
“How best to deliver glucose, both in terms of efficacy (e.g. resolution of symptoms and rate of normalisation of blood glucose levels) and safety (e.g. complications including aspiration), is unknown.….Buccal administration is defined as the application of glucose to the inner cheek mucosa; sublingual administration as the administration of glucose under the tongue; and both routes do not require swallowing of the glucose.” (1)
Respectfully,
UHMS HBO2 Safety Committee
REFERENCE/S: (Use for information necessary to identify and retrieve each work cited in the text above.)
- De Buck E, Borra V, Carlson JN, Zideman DA, Singletary EM, Djärv T. First aid glucose administration routes for symptomatic hypoglycaemia. Cochrane Database Syst Rev. 2019;4(4):CD013283. Published 2019 Apr 11.
- Heyboer Iii M, Wojcik SM, Swaby J, Boes T. Blood glucose levels in diabetic patients undergoing hyperbaric oxygen therapy. Undersea Hyperb Med. 2019;46(4):437-445.
- Marlowe N. Hyperbaric oxygen therapy and hypoglycemia in patients with diabetes. Wound Care Advantage. November 16, 2020. Accessed July 3, 2024.
- Nwafor TS. Managing Low Blood Glucose Levels in Patients Undergoing Hyperbaric Oxygen Therapy. Journal of Ostomy and Wound Management. Volume 60, Issue 4. April 1, 2014. Accessed July 3, 2024.
- Stevens SL, Sorita A, Narr AJ, et al. Applying quality improvement methods in a hyperbaric oxygen program: reducing unnecessary glucose testing. Undersea Hyperb Med. 2016;43(4):427-435.
BIBLIOGRAPHY: (Use for background or further reading.)
- Best Publishing Company. Hyperbaric Nursing and Wound Care. Flagstaff: Best Publishing Company; 2010.
- Huang HT. Hyperbaric Oxygen Therapy Indications. 15th ed.: Best Publishing Company; 2023.
- Whelan HT, Kindwall EP. Hyperbaric Medicine Practice, 4th ed.: Best Publishing Company; 2017.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members can provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and hyperbaric safety director/coordinator of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
